Music Therapy and Psychoneuroimmunological Markers in Children With Chronic Disease: A Systematic Review
DOI:
https://doi.org/10.23917/bik.v18i1.7517Keywords:
biomarkers; chronic disease; music therapy; pediatrics; psychoneuroimmunologyAbstract
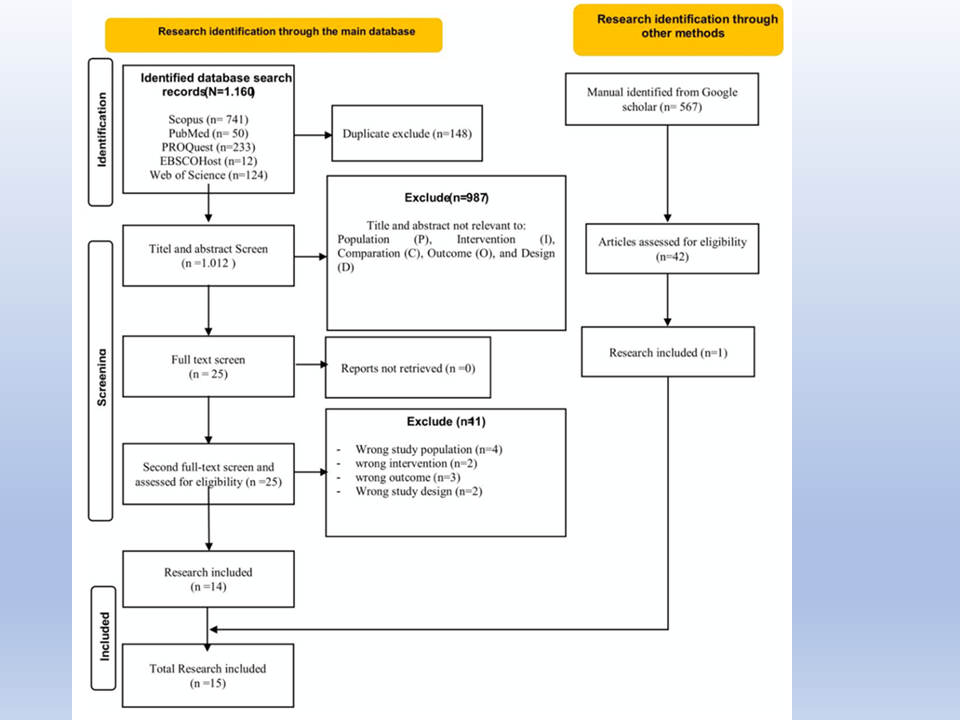
Stress conditions in children with chronic disease affect psychoneuroimmunological markers. One of the mind-body modalities commonly used in pediatric chronic disease is music therapy. This systematic aim was evaluating the effect of music therapy on psychoneuroimmunological markers among children with chronic disease. Articles published between March 31, 2014, and April 1, 2023, were retrieved from five databases: Scopus, PubMed, Web of Science, EBSCOhost, and ProQuest. Rayyan, an AI-powered tool for systematic literature reviews, facilitated paper selection. Studies were screened based on pre-defined inclusion and exclusion criteria. The PRISMA checklist guided selection, and the JBI Critical Appraisal for quality assessment. Data analysis employed a descriptive approach. A total of 15 articles published between 2014 and 2023 were included in this review. 10 (66,7%) of 15 studies assessed the effectiveness of music therapy on psychological and physiological responses. Meanwhile, five (33,3%) studies assessed the effectiveness of music therapy on neuroimmunological markers. Among the five studies, one did not exhibit a statistically significant impact. In contrast, the remaining four studies displayed a significant impact of music therapy on neuroimmunological markers. The most studies assessed the impact of music therapy on psychological and physiological responses, but only a small proportion assessed the effectiveness of music therapy on neuroimmunological markers. Music therapy can be considered a safe and generally well-accepted intervention in pediatric health care to manage psychoneuroimmunological markers.
Downloads
References
Abd-Elshafy, S. K., Khalaf, G. S., Abo-Kerisha, M. Z., Ahmed, N. T., El-Aziz, M. A. A., & Mohamed, M. A. (2015). Not All Sounds Have Negative Effects on Children Undergoing Cardiac Surgery. Journal of Cardiothoracic and Vascular Anesthesia, 29(5), 1277–1284. https://doi.org/10.1053/j.jvca.2015.01.005 DOI: https://doi.org/10.1053/j.jvca.2015.01.005
Anderson, E., & Durstine, J. L. (2019). Physical activity, exercise, and chronic diseases: A brief review. Sports Medicine and Health Science, 1(1), 3–10. https://doi.org/10.1016/j.smhs.2019.08.006 PubMed: PMID: 35782456 DOI: https://doi.org/10.1016/j.smhs.2019.08.006
Asnidar, Haerati, & Hilmi Nurfadillah. (2018). Description Of Hospitalization Stress Of Children’s Age Pre-School. Comprehensive Health Care, 2(3), 117–123. https://doi.org/10.37362/jch.v2i3.251 DOI: https://doi.org/10.37362/jch.v2i3.251
Atiwannapat, P., Thaipisuttikul, P., Poopityastaporn, P., & Katekaew, W. (2016). Active versus receptive group music therapy for major depressive disorder-A pilot study. Complementary Therapies in Medicine, 26, 141–145. https://doi.org/10.1016/j.ctim.2016.03.015 PubMed: PMID: 27261995 DOI: https://doi.org/10.1016/j.ctim.2016.03.015
Atiye Karakul, Esra Ardahan Akgul, Reyhan Yaliniz;, T. M. (2022). Effectiveness of music during cardiac catheterization on children’s pain, fear, anxiety and vital signs: A randomized, blind controlled trial. Journal Pediatric Nursing, 65, e56–e62. DOI: https://doi.org/10.1016/j.pedn.2022.02.009
CDC. (2021). About Chronic Diseases. Centers for Disease Control and Prevention. https://www.cdc.gov/chronic-disease/about/index.html
Chacin-Fernández, J., Chacin Fuenmayor, M., Piñerua-Shuhaibar, L., & Suarez-Roca, H. (2019). Psychological intervention based on psychoneuroimmunology improves clinical evolution, quality of life, and immunity of children with leukemia: A preliminary study. Health Psychology Open, 6(1). https://doi.org/10.1177/2055102919838902 PubMed: PMID: 30967959 DOI: https://doi.org/10.1177/2055102919838902
Chahal, J. K., Sharma, P., Sulena, & Rawat, H. C. L. (2021). Effect of music therapy on ICU induced anxiety and physiological parameters among ICU patients: An experimental study in a tertiary care hospital of India. Clinical Epidemiology and Global Health, 11(February), 100716. https://doi.org/10.1016/j.cegh.2021.100716 DOI: https://doi.org/10.1016/j.cegh.2021.100716
Compas, B. E., Jaser, S. S., Dunn, M. J., & Rodriguez, E. M. (2012). Coping with chronic illness in childhood and adolescence. Annual Review of Clinical Psychology, 8, 455–480. https://doi.org/10.1146/annurev-clinpsy-032511-143108 PubMed: PMID: 22224836 DOI: https://doi.org/10.1146/annurev-clinpsy-032511-143108
Cumpston, M. S., McKenzie, J. E., Thomas, J., & Brennan, S. E. (2021). The use of “PICO for synthesis” and methods for synthesis without meta-analysis: Protocol for a survey of current practice in systematic reviews of health interventions. F1000Research, 9, 1–26. https://doi.org/10.12688/f1000research.24469.2 PubMed: PMID: 33728041 DOI: https://doi.org/10.12688/f1000research.24469.2
Dantzer, R. (2018). Neuroimmune interactions: From the brain to the immune system and vice versa. Physiological Reviews, 98(1), 477–504. https://doi.org/10.1152/physrev.00039.2016 PubMed: PMID: 29351513 DOI: https://doi.org/10.1152/physrev.00039.2016
El-Farhan, N., Rees, D. A., & Evans, C. (2017). Measuring cortisol in serum, urine and saliva – are our assays good enough? Annals of Clinical Biochemistry, 54(3), 308–322. https://doi.org/10.1177/0004563216687335 PubMed: PMID: 28068807 DOI: https://doi.org/10.1177/0004563216687335
Fancourt, D., Ockelford, A., & Belai, A. (2014). The psychoneuroimmunological effects of music: A systematic review and a new model. Brain, Behavior, and Immunity, 36, 15–26. https://doi.org/10.1016/j.bbi.2013.10.014 PubMed: PMID: 24157429 DOI: https://doi.org/10.1016/j.bbi.2013.10.014
Finn, S., & Fancourt, D. (2018). The biological impact of listening to music in clinical and nonclinical settings: A systematic review. In Progress in Brain Research (1st ed., Vol. 237). Elsevier B.V. https://doi.org/10.1016/bs.pbr.2018.03.007 DOI: https://doi.org/10.1016/bs.pbr.2018.03.007
Furlan JC, Singh J, Hsieh J, et al. (2011). Reviews Methodology of Systematic Reviews and Recommendations. DOI: https://doi.org/10.1089/neu.2009.1146
Giordano, F., Zanchi, B., De Leonardis, F., Rutigliano, C., Esposito, F., Brienza, N., & Santoro, N. (2020). The influence of music therapy on preoperative anxiety in pediatric oncology patients undergoing invasive procedures. Arts in Psychotherapy, 68(October 2019), 101649. https://doi.org/10.1016/j.aip.2020.101649 DOI: https://doi.org/10.1016/j.aip.2020.101649
Gok Ugur, H., Yaman Aktaş, Y., Orak, O. S., Saglambilen, O., & Aydin Avci, İ. (2017). The effect of music therapy on depression and physiological parameters in elderly people living in a Turkish nursing home: a randomized-controlled trial. Aging and Mental Health, 21(12), 1280–1286. https://doi.org/10.1080/13607863.2016.1222348 PubMed: PMID: 27592520 DOI: https://doi.org/10.1080/13607863.2016.1222348
Gold, C., Solli, H. P., Krüger, V., & Lie, S. A. (2009). Dose-response relationship in music therapy for people with serious mental disorders: Systematic review and meta-analysis. Clinical Psychology Review, 29(3), 193–207. https://doi.org/10.1016/j.cpr.2009.01.001 PubMed: PMID: 19269725 DOI: https://doi.org/10.1016/j.cpr.2009.01.001
Gomez-Gallego, M., Gómez-Gallego, J. C., Gallego-Mellado, M., & García-García, J. (2021). Comparative efficacy of active group music intervention versus group music listening in alzheimer’s disease. International Journal of Environmental Research and Public Health, 18(15). https://doi.org/10.3390/ijerph18158067 PubMed: PMID: 34360360 DOI: https://doi.org/10.3390/ijerph18158067
Gonzalez-Díaz, S. N., Arias-Cruz, A., Elizondo-Villarreal, B., & Monge-Ortega, O. P. (2017). Psychoneuroimmunoendocrinology: clinical implications. World Allergy Organization Journal, 10(1), 19. https://doi.org/10.1186/s40413-017-0151-6 PubMed: PMID: 28616124 DOI: https://doi.org/10.1186/s40413-017-0151-6
Hasanah, I., Nursalam, N., Krisnana, I., Ramdani, W. F., Haikal, Z., & Rohita, T. (2023). Psychoneuroimmunological Markers of Psychological Intervention in Pediatric Cancer: A Systematic Review and New Integrative Model. Asian Nursing Research, 17(3), 119–137. https://doi.org/10.1016/j.anr.2023.07.001 PubMed: PMID: 37499937 DOI: https://doi.org/10.1016/j.anr.2023.07.001
Hasanah, I., Mulatsih, S., Haryanti, F., & Haikal, Z. (2020). Effect of music therapy on cortisol as a stress biomarker in children undergoing IV-line insertion. Journal of Taibah University Medical Sciences, 15(3), 238–243. https://doi.org/10.1016/j.jtumed.2020.03.007 DOI: https://doi.org/10.1016/j.jtumed.2020.03.007
Huang, Y. L., Lei, Y. Q., Liu, J. F., Cao, H., Yu, X. R., & Chen, Q. (2021). The music video therapy in postoperative analgesia in preschool children after cardiothoracic surgery. Journal of Cardiac Surgery, 36(7), 2308–2313. https://doi.org/10.1111/jocs.15551 DOI: https://doi.org/10.1111/jocs.15551
Huang, Y. L., Xu, N., Huang, S. T., Wang, Z. C., Cao, H., Yu, X. R., & Chen, Q. (2021). Impact of Music Therapy on Preoperative Anxiety and Degree of Cooperation With Anesthesia Induction in Children With Simple Congenital Heart Disease. Journal of Perianesthesia Nursing, 36(3), 243–246. https://doi.org/10.1016/j.jopan.2020.08.004 DOI: https://doi.org/10.1016/j.jopan.2020.08.004
Iqbal, T., Elahi, A., Wijns, W., & Shahzad, A. (2023). Cortisol detection methods for stress monitoring in connected health. Health Sciences Review, 6(January), 100079. https://doi.org/10.1016/j.hsr.2023.100079 DOI: https://doi.org/10.1016/j.hsr.2023.100079
Josephine Geipel, Julian Koenig, Thomas K. Hillecke, F. R. (2022). Short-term music therapy treatment for adolescents with depression – A pilot study. The Arts in Psychotherapy. https://doi.org/10.1016/j.aip.2021.101874 DOI: https://doi.org/10.1016/j.aip.2021.101874
King, E. (2017). Chronic Illnes and Functionality: How it affects adolescents academically and socially and how they can cope. Institution: The BYU Undergraduate Journal in Psychology, 12(2), 94–106. https://scholarsarchive.byu.edu/intuition/vol12/iss2/8
Kobus, S., Buehne, A. M., Kathemann, S., Buescher, A. K., & Lainka, E. (2022). Effects of Music Therapy on Vital Signs in Children with Chronic Disease. International Journal of Environmental Research and Public Health, 19(11). https://doi.org/10.3390/ijerph19116544 DOI: https://doi.org/10.3390/ijerph19116544
Kuhlmann, A. Y. R., Van Rosmalen, J., Staals, L. M., Keyzer-Dekker, C. M. G., Dogger, J., De Leeuw, T. G., Van Der Toorn, F., Jeekel, J., Wijnen, R. M. H., & Van Dijk, M. (2020). Music interventions in pediatric surgery (The music under surgery in children study): A randomized clinical trial. Anesthesia and Analgesia, 130(4), 991–1001. https://doi.org/10.1213/ANE.0000000000003983 DOI: https://doi.org/10.1213/ANE.0000000000003983
Lee, D. Y., Kim, E., & Choi, M. H. (2015). Technical and clinical aspects of cortisol as a biochemical marker of chronic stress. BMB Reports, 48(4), 209–216. https://doi.org/10.5483/BMBRep.2015.48.4.275 PubMed: PMID: 25560699 DOI: https://doi.org/10.5483/BMBRep.2015.48.4.275
Li, Y., Xing, X., Shi, X., Yan, P., Chen, Y., Li, M., Zhang, W., Li, X., & Yang, K. (2020). The effectiveness of music therapy for patients with cancer: A systematic review and meta-analysis. Journal of Advanced Nursing, 76(5), 1111–1123. https://doi.org/10.1111/jan.14313 PubMed: PMID: 32017183 DOI: https://doi.org/10.1111/jan.14313
Lieber, A. C., Bose, J., Zhang, X., Seltzberg, H., Loewy, J., Rossetti, A., Mocco, J., & Kellner, C. P. (2019). Effects of music therapy on anxiety and physiologic parameters in angiography: A systematic review and meta-analysis. Journal of NeuroInterventional Surgery, 11(4), 416–431. https://doi.org/10.1136/neurintsurg-2018-014313 PubMed: PMID: 30415224 DOI: https://doi.org/10.1136/neurintsurg-2018-014313
Linda L. Chlan et al. (2013). Effects of patient-directed music intervention on anxiety and sedative exposure in critically ill patients receiving mechanical- ventilatory support: a randomized clinical trial. Nih, 23(1), 1–7. https://doi.org/10.1001/jama.2013.5670 PubMed: PMID: 23689789
Majid, U. (2018). Research Fundamentals: Study Design, Population, and Sample Size. Undergraduate Research in Natural and Clinical Science and Technology (URNCST) Journal, 2, 1–7. https://doi.org/10.26685/urncst.16 DOI: https://doi.org/10.26685/urncst.16
Millett, C. R., & Gooding, L. F. (2017). Comparing active and passive distraction-based music therapy interventions on preoperative anxiety in pediatric patients and their caregivers. Journal of Music Therapy, 54(4), 460–478. https://doi.org/10.1093/jmt/thx014 PubMed: PMID: 29253180 DOI: https://doi.org/10.1093/jmt/thx014
Noushad Shamoon, Ahmed Sadaf, Ansari Basit, Mustafa Umme-Hani, Saleem Yusra, & Hazrat Hina. (2021). Physiological biomarkers of chronic stress: A systematic review Introduction. International Journal Of Health Sciences, 15(5), 46–59. PubMed: PMID: 34548863
Oakley, R. H., & Cidlowski, J. A. (2013). The biology of the glucocorticoid receptor: New signaling mechanisms in health and disease. Journal of Allergy and Clinical Immunology, 132(5), 1033–1044. https://doi.org/10.1016/j.jaci.2013.09.007 PubMed: PMID: 24084075 DOI: https://doi.org/10.1016/j.jaci.2013.09.007
Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan-a web and mobile app for systematic reviews. Systematic Reviews, 5(1), 1–10. https://doi.org/10.1186/s13643-016-0384-4 DOI: https://doi.org/10.1186/s13643-016-0384-4
Page, M. J., Moher, D., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., Mcdonald, S., … Mckenzie, J. E. (2021). PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. The BMJ, 372. https://doi.org/10.1136/bmj.n160 DOI: https://doi.org/10.1136/bmj.n160
Park, J. I., Lee, I. H., Lee, S. J., Kwon, R. W., Choo, E. A., Nam, H. W., & Lee, J. B. (2023). Effects of music therapy as an alternative treatment on depression in children and adolescents with ADHD by activating serotonin and improving stress coping ability. BMC Complementary Medicine and Therapies, 23(1), 1–14. https://doi.org/10.1186/s12906-022-03832-6 DOI: https://doi.org/10.1186/s12906-022-03832-6
Roslita, R., Nurhaeni, N., & Wanda, D. (2017). The Effects of Music Therapy on the Physiological Response of Asthmatic Children Receiving Inhalation Therapy. Comprehensive Child and Adolescent Nursing, 40(1), 45–51. https://doi.org/10.1080/24694193.2017.1386970 DOI: https://doi.org/10.1080/24694193.2017.1386970
Sai Prashanti Gumpili & Anthony Vipin Das. (2022). Sample size and its evolution in research. IHOPE Journal of Ophthalmology Review, 1(2), 9–13. https://doi.org/10.25259/IHOPEJO_3_2021 DOI: https://doi.org/10.25259/IHOPEJO_3_2021
Polat (2015). The effect of therapeutic music on anxiety in children with acute lymphoblastic leukaemia.
Sheikhi, A. R., Naderifar, M., Abdollahimohammad, A., Mohammad, A. A., Mastalizadeh, H., & Sheikhi, H. R. (2020). The Effect of Music Therapy on the Anxiety Level of Children with Thalassemia Major under Blood Transfusion. Archives of Pharmacy Practice, 11(4), 66–69.
Sittler, M. C., Worschech, F., Wilz, G., Fellgiebel, A., & Wuttke-Linnemann, A. (2021). Psychobiological mechanisms underlying the health-beneficial effects of music in people living with dementia: A systematic review of the literature. Physiology and Behavior, 233(September 2020), 113338. https://doi.org/10.1016/j.physbeh.2021.113338 PubMed: PMID: 33497696 DOI: https://doi.org/10.1016/j.physbeh.2021.113338
Slopen, N., McLaughlin, K. A., & Shonkoff, J. P. (2014). Interventions to improve cortisol regulation in children: A systematic review. Pediatrics, 133(2), 312–326. https://doi.org/10.1542/peds.2013-1632 PubMed: PMID: 24420810 DOI: https://doi.org/10.1542/peds.2013-1632
Sophia M. Foroushani, Cade A. Herman, Carlie A. Wiseman, Chandler M. Anthony, Stacy S. Drury, M. P. H. (2020). Effects of music therapy on anxiety and physiologic parameters in angiography: A systematic review and meta-analysis. Journal of Perinatology, 40, 1770–1779. DOI: https://doi.org/10.1038/s41372-020-0756-4
Taets, G. G. D. C., Jomar, R. T., Abreu, A. M. M., & Capella, M. A. M. (2019). Effect of music therapy on stress in chemically dependent people: A quasi-experimental study. Revista Latino-Americana de Enfermagem, 27. https://doi.org/10.1590/1518-8345.2456.3115 PubMed: PMID: 30698217 DOI: https://doi.org/10.1590/1518-8345.2456.3115
Tawfik, G. M., Dila, K. A. S., Mohamed, M. Y. F., Tam, D. N. H., Kien, N. D., Ahmed, A. M., & Huy, N. T. (2019). A step by step guide for conducting a systematic review and meta-analysis with simulation data. Tropical Medicine and Health, 47(1), 1–9. https://doi.org/10.1186/s41182-019-0165-6 PubMed: PMID: 31388330 DOI: https://doi.org/10.1186/s41182-019-0165-6
Ting-Ting Zhang , Zhong Fan , Shu-Zhen Xu Zheng-Yao Guo , Min Cai , Qiong Li , Yan-Lai Tang , Li-Wei Wang , Xi Chen , Li-Jun Tang , Zhi-Ying Li, Y. W. (2023). The effects of music therapy on peripherally inserted central catheter in hospitalized children with leukemia. J Psychosoc Oncol, 41, 76–86. DOI: https://doi.org/10.1080/07347332.2022.2044967
Uggla, L., Bonde, L. O., Svahn, B. M., Remberger, M., Wrangsjö, B., & Gustafsson, B. (2016). Music therapy can lower the heart rates of severely sick children. Acta Paediatrica, International Journal of Paediatrics, 105(10), 1225–1230. https://doi.org/10.1111/apa.13452 DOI: https://doi.org/10.1111/apa.13452
U N Ijoma , N N Unaogu , T I Onyeka , C B Nwatu , C L Onyekonwu , I O Onwuekwe , F Ugwumba , R C Nwutobo, C. V. N. (2019). Health-related quality of life in people with chronic diseases managed in a low-resource setting - A study from South East Nigeria. Niger J Clin Pract, 22(9). https://doi.org/https://doi.org/10.4103/njcp.njcp_29_19 PubMed: PMID: 31489851 DOI: https://doi.org/10.4103/njcp.njcp_29_19
White, G. E., Caterini, J. E., McCann, V., Rendall, K., Nathan, P. C., Rhind, S. G., Jones, H., & Wells, G. D. (2021). The psychoneuroimmunology of stress regulation in pediatric cancer patients. Cancers, 13(18), 1–23. https://doi.org/10.3390/cancers13184684 PubMed: PMID: 34572911 DOI: https://doi.org/10.3390/cancers13184684
Yan, Q. (2016). Psychoneuroimmunology: Systems Biology Approaches to Mind-Body Medicine. Epub Ahead of Print 2016. https://doi.org/10.1007/978-3-319-45111-4.
Yinger, O. S., & Gooding, L. (2014). Music therapy and music medicine for children and adolescents. Child and Adolescent Psychiatric Clinics of North America, 23(3), 535–553. https://doi.org/10.1016/j.chc.2013.03.003 PubMed: PMID: 24975624 DOI: https://doi.org/10.1016/j.chc.2013.03.003
Zhang, J. M., Wang, P., Yao, J. X., Zhao, L., Davis, M. P., Walsh, D., & Yue, G. H. (2012). Music interventions for psychological and physical outcomes in cancer: A systematic review and meta-analysis. Supportive Care in Cancer, 20(12), 3043–3053. https://doi.org/10.1007/s00520-012-1606-5 PubMed: PMID: 23052912 DOI: https://doi.org/10.1007/s00520-012-1606-5
Ziba Vaghri, Jean Zermatten, Gerison Lansdown, R. R. (2022). Monitoring State Compliance with the UN Convention on the Rights of the Child. In Cham: Springer International Publishing. https://doi.org/10.1007/978-3-030-84647-3
Submitted
Accepted
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Idyatul Hasanah, Chui Ping Lei, Zikrul Haikal, Apriani Susmita Sari, Domingos Soares, Kurniati Prihatin

This work is licensed under a Creative Commons Attribution 4.0 International License.


















