Health Challenges Experienced by Widows in Low- and Middle-Income Countries: A Systematic Review
DOI:
https://doi.org/10.23917/indigenous.v9i3.5684Keywords:
Chronic diseases, Health problems, Psychological adaptation, Depression, LonelinessAbstract
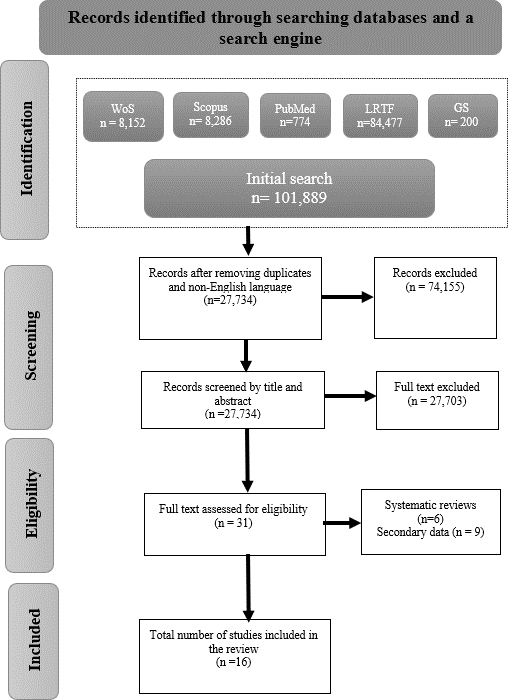
This systematic review aims to critically examine empirical studies conducted in low- and middle-income countries (LMICs) to identify and analyze the diverse health challenges widows face. Specifically, the review aims to explore the psychological factors impacting their well-being and assess these challenges' implications for health outcomes. The research encompassed articles published between 2012 and 2024, sourced from PubMed, Web of Science, Scopus, and Taylor and Francis databases and the Google Scholar search engine. A total 101,889 papers were initially screened, ultimately culminating in the inclusion of sixteen papers following a meticulous evaluation and screening process. The findings revealed that widows commonly experience health challanges. In this review health challenges is presented into two major themes: mental health challenges such as depression, anxiety and stress, often stemming from emotional distress and social isoloation. The other theme is the physical health challenges that indicates a high prevalence of chronic diseases and malnutrition duet o financial instability. The study also identified several psychological factors, notably finansial insecurity, contributing to heightened stress and anxiety, further complicating their mental health. Many widows also face diminished social support leading to increased feelings of loneliness and stigma, while economic hardship significantly limits their access to healthcare and basic needs. Overall, these findings highlight the complex interplay of mental, physical and social factors, including critical psychological dimensions that affects the well-being of widows worldwide. This review was registered as PROSPERO 2022 CRD42022382703 with minor modifications.
References
Adena, M., Hamermesh, D., Myck, M., & Oczkowska, M. (2023). Home alone: Widows’ well-being and time. Journal of Happiness Studies, 24(2), 813–838. https://doi.org/10.1007/s10902-023-00622-w DOI: https://doi.org/10.1007/s10902-023-00622-w
Agboeze, M. U., Nwachukwu, R. U., Ugwueze, M. O., & Agboeze, M. N. (2020). Health status of widows as a correlate of their participation in community development projects in Nsukka, Enugu State, Nigeria. Global Journal of Health Science, 12(7), 72. https://doi.org/10.5539/gjhs.v12n7p72 DOI: https://doi.org/10.5539/gjhs.v12n7p72
Agrawal, G., & Arokiasamy, P. (2010). Morbidity prevalence and health care utilization among older adults in India. Journal of Applied Gerontology, 29(2), 155–179. https://doi.org/10.1177/0733464809339622 DOI: https://doi.org/10.1177/0733464809339622
Agrawal, G., & Keshri, K. (2014). Morbidity patterns and health care seeking behavior among older widows in India. PLoS ONE, 9(4), e94295. https://doi.org/10.1371/journal.pone.0094295 DOI: https://doi.org/10.1371/journal.pone.0094295
Akpalaba, I. O., Blackie, F. F., & Akpalaba, R. U. E. (2021). Community health services: Impact on geriatrics and widows. Advances in Research, 22(3), 30–41. https://doi.org/10.9734/air/2021/v22i330302 DOI: https://doi.org/10.9734/air/2021/v22i330302
Avison, W. R., Ali, J., & Walters, D. (2007). Family structure, stress, and psychological distress: A demonstration of the impact of differential exposure. Journal of Health and Social Behavior, 48(3), 301–317. https://doi.org/10.1177/002214650704800307 DOI: https://doi.org/10.1177/002214650704800307
Burns, R. A., Browning, C. J., & Kendig, H. L. (2015). Examining the 16-year trajectories of mental health and wellbeing through the transition into widowhood. International Psychogeriatrics, 27(12), 1979–1986. https://doi.org/10.1017/S1041610215000472 DOI: https://doi.org/10.1017/S1041610215000472
Busari, A. O., & Folaranmi, O. O. (2014). An empirical inquiry to psychological variables constituting stress: Middle-aged widows in rural communities in Nigeria. The Journal of Pan African Studies, 7(3), 210–222.
Carey, M., Small, H., Yoong, S. L., Boyes, A., Bisquera, A., & Sanson-Fisher, R. (2014). Prevalence of comorbid depression and obesity in general practice: A cross-sectional survey. British Journal of General Practice, 64(620), e122–e127. https://doi.org/10.3399/bjgp14X677482 DOI: https://doi.org/10.3399/bjgp14X677482
Carr, D., & Bodnar-Deren, S. (2009). Gender, aging, and widowhood. In P. Uhlenberg (Ed.), International handbook of population aging (pp. 705–728). Springer. https://doi.org/10.1007/978-1-4020-8356-3_28 DOI: https://doi.org/10.1007/978-1-4020-8356-3_32
CASP. (2014). Critical Appraisal Skills Programme (CASP) checklist. https://www.gla.ac.uk/media/media_64047_en.pdf
Centers for Disease Control and Prevention (CDC). (2016). Chronic disease overview. https://www.cdc.gov/chronicdisease/overview/index.htm
Cheng, S.-T., Chan, T. W. S., Li, G. H. K., & Leung, E. M. F. (2014). Childlessness and subjective well-being in Chinese widowed persons. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 69B(1), 48–52. https://doi.org/10.1093/geronb/gbt049 DOI: https://doi.org/10.1093/geronb/gbt049
Cochran, A. L., McDonald, N. C., Prunkl, L., Vinella-Brusher, E., Wang, J., Oluyede, L., & Wolfe, M. (2022). Transportation barriers to care among frequent health care users during the COVID pandemic. BMC Public Health, 22(1), 1783. https://doi.org/10.1186/s12889-022-14149-x DOI: https://doi.org/10.1186/s12889-022-14149-x
Daoulah, A., Al-Murayeh, M., Al-kaabi, S., Lotfi, A., Elkhateeb, O. E., Al-Faifi, S. M., Alqahtani, S., Stewart, J., Heavey, J., Hurley, W. T., Alama, M. N., Faden, M., Al-Shehri, M., Youssef, A., & Alsheikh-Ali, A. A. (2017). Divorce and severity of coronary artery disease: A multicenter study. Cardiology Research and Practice, 2017, 1–8. https://doi.org/10.1155/2017/4751249 DOI: https://doi.org/10.1155/2017/4751249
Das, A. (2012). Spousal loss and health in late life: Moving beyond emotional trauma. Journal of Aging and Health, 25(2), 221–245. https://doi.org/10.1177/0898264312464498 DOI: https://doi.org/10.1177/0898264312464498
De Vries, B., Utz, R., Caserta, M., & Lund, D. (2014). Friend and family contact and support in early widowhood. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 69B(1), 75–84. https://doi.org/10.1093/geronb/gbt078 DOI: https://doi.org/10.1093/geronb/gbt078
DiGiacomo, M., Lewis, J., Nolan, M. T., Phillips, J., & Davidson, P. M. (2013). Health transitions in recently widowed older women: A mixed methods study. BMC Health Services Research, 13(1), 143. https://doi.org/10.1186/1472-6963-13-143 DOI: https://doi.org/10.1186/1472-6963-13-143
Dube, M. (2022). Isolation and its impact on widows: Insights from low-resourced communities in Binga District, Zimbabwe. Social Sciences, 11(7), 298. https://doi.org/10.3390/socsci11070298 DOI: https://doi.org/10.3390/socsci11070298
Ebulum, G. C., Eze, J. E., Ezeihuoma, O. P., Njoku, C., & Chukwuorji, J. C. (2024). Roles of loneliness, stress, and religiosity in suicide ideation among Nigerian older adults. The International Journal of Aging and Human Development, 00914150241268006. https://doi.org/10.1177/00914150241268006 DOI: https://doi.org/10.1177/00914150241268006
Ezeh, V. C. (2022). Post-traumatic stress disorder among rural widows in Nsukka: Risk factors and wellbeing domains. South African Journal of Psychology, 52(2), 202–213. https://doi.org/10.1177/00812463211040378 DOI: https://doi.org/10.1177/00812463211040378
Freak-Poli, R., Kung, C. S. J., Ryan, J., & Shields, M. A. (2022). Social isolation, social support, and loneliness profiles before and after spousal death and the buffering role of financial resources. The Journals of Gerontology: Series B, 77(5), 956–971. https://doi.org/10.1093/geronb/gbac039 DOI: https://doi.org/10.1093/geronb/gbac039
Gillies, J., & Neimeyer, R. A. (2006). Loss, grief, and the search for significance: Toward a model of meaning reconstruction in bereavement. Journal of Constructivist Psychology, 19(1), 31–65. https://doi.org/10.1080/10720530500311182 DOI: https://doi.org/10.1080/10720530500311182
Golden, J., Conroy, R. M., Bruce, I., Denihan, A., Greene, E., Kirby, M., & Lawlor, B. A. (2009). Loneliness, social support networks, mood and wellbeing in community-dwelling elderly. International Journal of Geriatric Psychiatry, 24(7), 694–700. https://doi.org/10.1002/gps.2181 DOI: https://doi.org/10.1002/gps.2181
Halleröd, B., & Gustafsson, J.-E. (2011). A longitudinal analysis of the relationship between changes in socio-economic status and changes in health. Social Science & Medicine, 72(1), 116–123. https://doi.org/10.1016/j.socscimed.2010.09.036 DOI: https://doi.org/10.1016/j.socscimed.2010.09.036
Hamadeh, N., & Van Rompaey, C. (2023). World Bank Group country classifications by income level for FY24. https://blogs.worldbank.org/en/opendata/new-world-bank-group-country-classifications-income-level-fy24
Holm, A. L., Berland, A. K., & Severinsson, E. (2019). Factors that influence the health of older widows and widowers—A systematic review of quantitative research. Nursing Open, 6(2), 591–611. https://doi.org/10.1002/nop2.243 DOI: https://doi.org/10.1002/nop2.243
Jacobsen, J. C., Zhang, B., Block, S. D., Maciejewski, P. K., & Prigerson, H. G. (2010). Distinguishing symptoms of grief and depression in a cohort of advanced cancer patients. Death Studies, 34(3), 257–273. https://doi.org/10.1080/07481180903559303 DOI: https://doi.org/10.1080/07481180903559303
Jiang, C., Song, H., & Shi, J. (2023). The impact of widowhood on mental health of older adults. Geriatric Nursing, 50, 38–43. https://doi.org/10.1016/j.gerinurse.2022.12.019 DOI: https://doi.org/10.1016/j.gerinurse.2022.12.019
Kalantari, M., Zareei Mahmood Abadi, H., & Sedrpoushan, N. (2023). A qualitative study on prolonged grief for the loss of spouse in the COVID-19 pandemic: Exploring lived experience. Journal of Community Health Research. https://doi.org/10.18502/jchr.v12i6.12812 DOI: https://doi.org/10.18502/jchr.v12i6.12812
Kansra, P., & Khadar, A. A. (2023). Behavioural determinants of health-care utilisation among elderly population: A cross-sectional analysis from Punjab. Working with Older People, 1(1), 1–11. https://doi.org/10.1108/WWOP-05-2023-0018 DOI: https://doi.org/10.1108/WWOP-05-2023-0018
Keyes, K. M., Pratt, C., Galea, S., McLaughlin, K. A., Koenen, K. C., & Shear, M. K. (2014). The burden of loss: Unexpected death of a loved one and psychiatric disorders across the life course in a national study. American Journal of Psychiatry, 171(8), 864–871. https://doi.org/10.1176/appi.ajp.2014.13081132 DOI: https://doi.org/10.1176/appi.ajp.2014.13081132
Kohl, C., McIntosh, E. J., Unger, S., Haddaway, N. R., Kecke, S., Schiemann, J., & Wilhelm, R. (2018). Online tools supporting the conduct and reporting of systematic reviews and systematic maps: A case study on CADIMA and review of existing tools. Environmental Evidence, 7(1), 8. https://doi.org/10.1186/s13750-018-0115-5 DOI: https://doi.org/10.1186/s13750-018-0115-5
Kolaski, K., Logan, L. R., & Ioannidis, J. P. A. (2023). Guidance to best tools and practices for systematic reviews. Systematic Reviews, 12(1), 96. https://doi.org/10.1186/s13643-023-02255-9 DOI: https://doi.org/10.1186/s13643-023-02255-9
Li, Y., Chan, W. C. H., Chen, H., & Ran, M. (2022). Widowhood and depression among Chinese older adults: Examining coping styles and perceptions of aging as mediators and moderators. Aging & Mental Health, 26(6), 1161–1169. https://doi.org/10.1080/13607863.2021.1935455 DOI: https://doi.org/10.1080/13607863.2021.1935455
Lloyd-Sherlock, P., Corso, B., & Minicuci, N. (2015). Widowhood, socio-economic status, health and wellbeing in low and middle-income countries. The Journal of Development Studies, 51(10), 1374–1388. https://doi.org/10.1080/00220388.2015.1066497 DOI: https://doi.org/10.1080/00220388.2015.1066497
Makgahlela, M. W., & Sodi, T. (2016). Cultural conceptions of a bereavement-related illness in a South African indigenous community. Journal of Psychology in Africa, 26(6), 541–545. https://doi.org/10.1080/14330237.2016.1250407 DOI: https://doi.org/10.1080/14330237.2016.1250407
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & The PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. https://doi.org/10.1371/journal.pmed.1000097 DOI: https://doi.org/10.1371/journal.pmed.1000097
Myroniuk, T. W. (2016). Marital dissolutions and the health of older individuals in a rural African context. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 72(4), 654–664. https://doi.org/10.1093/geronb/gbw077 DOI: https://doi.org/10.1093/geronb/gbw077
Nseir, S., & Larkey, L. K. (2013). Interventions for spousal bereavement in the older adult: An evidence review. Death Studies, 37(6), 495–512. https://doi.org/10.1080/07481187.2011.649941 DOI: https://doi.org/10.1080/07481187.2011.649941
Olawa, B. D., Omolayo, B. O., & Azikiwe, J. C. (2021). Gender influence on loneliness and family and nonfamily support among older adults: The confounding role of widowhood. Journal of Women & Aging, 33(3), 268–287. https://doi.org/10.1080/08952841.2019.1690370 DOI: https://doi.org/10.1080/08952841.2019.1690370
Oumer, B., Abera, R., Beshah, A., Tesfaye, S., Niguse, T., Mohammed, B., Yimer, A. A., & Sidamo, N. B. (2024). Prevalence of depressive symptoms and its associated factors among the aging population in Gamo zone, Southern Ethiopia: A community-based cross-sectional study. Frontiers in Psychiatry, 15, 1402622. https://doi.org/10.3389/fpsyt.2024.1402622 DOI: https://doi.org/10.3389/fpsyt.2024.1402622
Panagiotopoulos, G., Walker, R., & Luszcz, M. (2013). A comparison of widowhood and well-being among older Greek and British-Australian migrant women. Journal of Aging Studies, 27(4), 519–528. https://doi.org/10.1016/j.jaging.2013.03.005 DOI: https://doi.org/10.1016/j.jaging.2013.03.005
Perkins, J. M., Lee, H., James, K. S., Oh, J., Krishna, A., Heo, J., Lee, J., & Subramanian, S. V. (2016). Marital status, widowhood duration, gender and health outcomes: A cross-sectional study among older adults in India. BMC Public Health, 16(1), 1032. https://doi.org/10.1186/s12889-016-3682-9 DOI: https://doi.org/10.1186/s12889-016-3682-9
Polanco-Roman, L., Gomez, J., Miranda, R., & Jeglic, E. (2016). Stress-related symptoms and suicidal ideation: The roles of rumination and depressive symptoms vary by gender. Cognitive Therapy and Research, 40(5), 606–616. https://doi.org/10.1007/s10608-016-9782-0 DOI: https://doi.org/10.1007/s10608-016-9782-0
Polit, D. F., & Beck, C. T. (2012). Nursing research: Generating and assessing evidence for nursing practice. Wolters Kluwer Health.
Remillard, E. T., Campbell, M. L., Koon, L. M., & Rogers, W. A. (2022). Transportation challenges for persons aging with mobility disability: Qualitative insights and policy implications. Disability and Health Journal, 15(1), 101209. https://doi.org/10.1016/j.dhjo.2021.101209 DOI: https://doi.org/10.1016/j.dhjo.2021.101209
Ross, D. B., & Gale, J. (2021). The impact of family economic strain on work-family conflict, marital support, marital quality, and marital stability during the middle years. Journal of Family and Economic Issues, 42(4), 1–15. https://doi.org/10.1007/s10834-021-09782-4 DOI: https://doi.org/10.1007/s10834-021-09782-4
Ryu, S., & Fan, L. (2023). The relationship between financial worries and psychological distress among U.S. adults. Journal of Family and Economic Issues, 44(1), 16–33. https://doi.org/10.1007/s10834-022-09820-9 DOI: https://doi.org/10.1007/s10834-022-09820-9
Sandelowski, M. (2010). What’s in a name? Qualitative description revisited. Research in Nursing & Health, 33(1), 77–84. https://doi.org/10.1002/nur.20362 DOI: https://doi.org/10.1002/nur.20362
Schneider, Z., Whitehead, D., Elliott, D., Lobiondo-Wood, G., & Haber, J. (2007). Nursing and midwifery research: Methods and appraisal for evidence-based practice. Mosby Elsevier.
Sekgobela, G. L., Peu, D. M., & Van Der Wath, A. E. (2020). Health-support needs of widows in South Africa: A phenomenological inquiry. OMEGA - Journal of Death and Dying, 81(3), 507–522. https://doi.org/10.1177/0030222818786416 DOI: https://doi.org/10.1177/0030222818786416
Shafiq, S., Ullah, S., & Ayub, M. (2024). Socio-cultural challenges for widows: A case study in district Lahore, Punjab. Contemporary Issues in Social Sciences and Management Practices, 3(1), 245–256. https://doi.org/10.61503/cissmp.v3i1.139 DOI: https://doi.org/10.61503/cissmp.v3i1.139
Spahni, S., Morselli, D., Perrig-Chiello, P., & Bennett, K. M. (2015). Patterns of psychological adaptation to spousal bereavement in old age. Gerontology, 61(5), 456–468. https://doi.org/10.1159/000371444 DOI: https://doi.org/10.1159/000371444
Syed, S. T., Gerber, B. S., & Sharp, L. K. (2013). Traveling towards disease: Transportation barriers to health care access. Journal of Community Health, 38(5), 976–993. https://doi.org/10.1007/s10900-013-9681-1 DOI: https://doi.org/10.1007/s10900-013-9681-1
Szuhany, K. L., Malgaroli, M., Miron, C. D., & Simon, N. M. (2021). Prolonged grief disorder: Course, diagnosis, assessment, and treatment. Focus, 19(2), 161–172. https://doi.org/10.1176/appi.focus.20200052 DOI: https://doi.org/10.1176/appi.focus.20200052
Trivedi, J., Sareen, H., & Dhyani, M. (2009). Psychological aspects of widowhood and divorce. Mens Sana Monographs, 7(1), 37. https://doi.org/10.4103/0973-1229.40648 DOI: https://doi.org/10.4103/0973-1229.40648
Tshaka, A., Tanga, P., & Ntshongwana, Z. (2023). Socio-economic challenges experienced by widows and support provided by social workers in Raymond Mhlaba Local Municipality in Eastern Cape, South Africa. Southern African Journal of Social Work and Social Development, 35(3), 1–21. https://doi.org/10.25159/2708-9355/11179 DOI: https://doi.org/10.25159/2708-9355/11179
Williams, B. R., Sawyer, P., & Allman, R. M. (2012). Wearing the garment of widowhood: Variations in time since spousal loss among community-dwelling older adults. Journal of Women & Aging, 24(2), 126–139. https://doi.org/10.1080/08952841.2012.639660 DOI: https://doi.org/10.1080/08952841.2012.639660
Zheng, J., & Yan, L. (2024). The impact of widowhood on the mental health of older adults and the buffering effect of social capital. Frontiers in Public Health, 12, 1385592. https://doi.org/10.3389/fpubh.2024.1385592 DOI: https://doi.org/10.3389/fpubh.2024.1385592
Zhou, J., & Hearst, N. (2016). Health-related quality of life among elders in rural China: The effect of widowhood. Quality of Life Research, 25(12), 3087–3095. https://doi.org/10.1007/s11136- DOI: https://doi.org/10.1007/s11136-016-1338-y
Submitted
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Neema Florence Vincent Mosha, Patrick Ngulube

This work is licensed under a Creative Commons Attribution 4.0 International License.











