Phenomenology Study: Occupational Diseases and Accidents in Nurses in Coastal and Border Areas
DOI:
https://doi.org/10.23917/bik.v18i1.6840Keywords:
Nurses, Occupational Diseases, Occupational Accidents, Border Areas, Coastal AreasAbstract
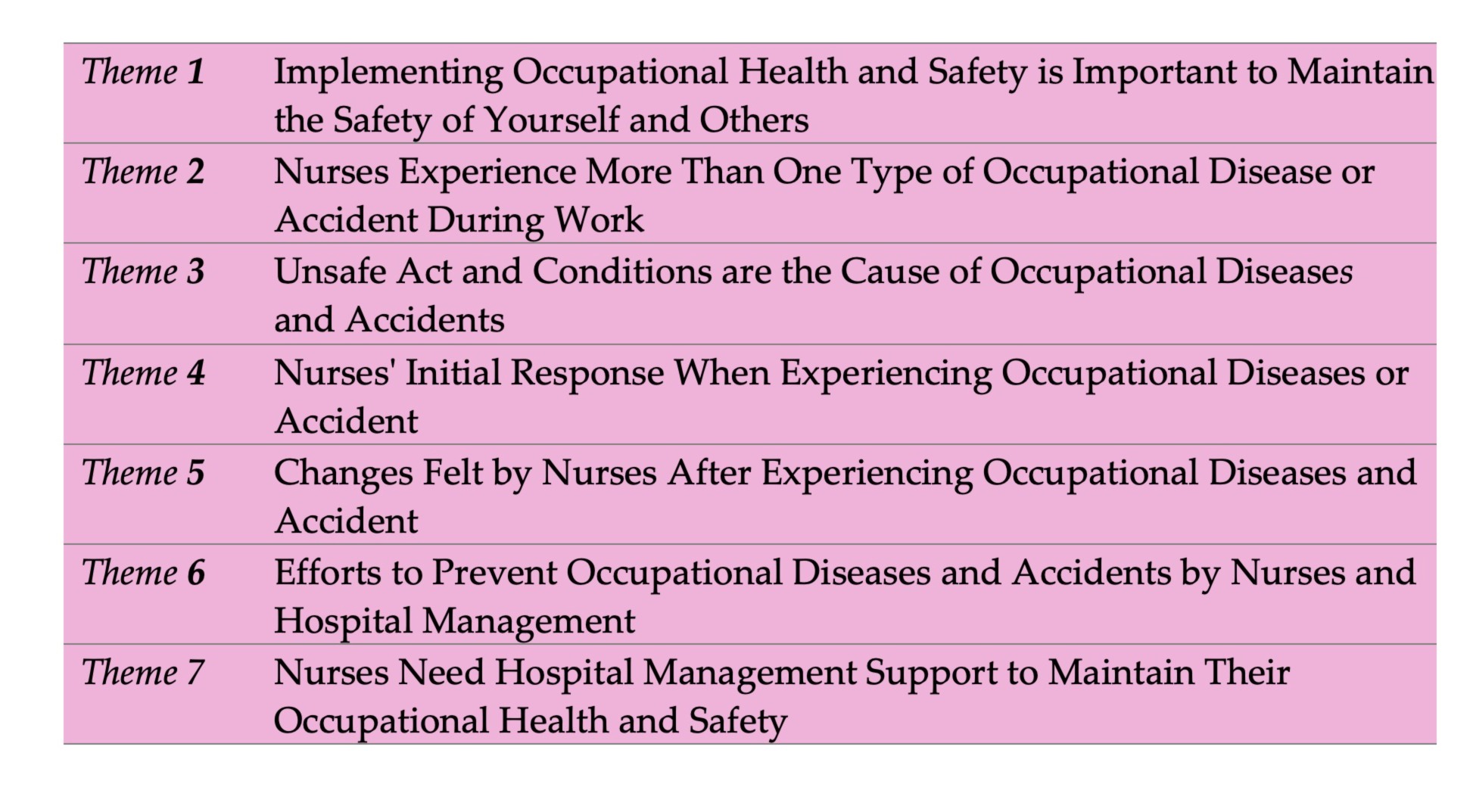
Nurses are health workers who are at high risk of experiencing occupational diseases and accidents. The purpose of this study was to obtain an overview of the experiences of nurses in coastal and border areas who have experienced occupational diseases or accidents. This study used a qualitative design with a phenomenological method. Participants were selected using purposive sampling techniques of 9 nurses from different rooms. Data were collected using in-depth interviews related to experiences. 7 themes were identified in this study, namely: 1)Implementing Occupational Health and Safety is Important to Maintain the Safety of Yourself and Others. 2) Nurses experience more than one type of occupational disease or accident during work. 3) Unsafe acts and conditions are the causes of occupational diseases and accidents. 4) Nurses’ initial response when experiencing occupational diseases or accidents. 5) Changes felt by nurses after experiencing occupational diseases and accidents. 6) Efforts to prevent occupational diseases and accidents by nurses and hospital management. 7) Nurses need Hospital Management support to maintain their Occupational Health and Safety. Conclusion: occupational diseases and accidents can be caused by the negligence of nurses themselves, co-workers, patients, and patient companions, the lack of managerial roles, and an unsafe environment. Experience of work accidents causes physical and psychological discomfort in nurses which can be temporary or long-term. Therefore, support from all parties is needed to maintain Occupational Health and Safety for nurses.
Downloads
References
Abbas, M., Robalo Nunes, T., Martischang, R., Zingg, W., Iten, A., Pittet, D., & Harbarth, S. (2021). Nosocomial transmission and outbreaks of coronavirus disease 2019: The need to protect both patients and healthcare workers. Antimicrobial Resistance and Infection Control, 10(1), 1–13. https://doi.org/10.1186/s13756-020-00875-7
Afiyanti, Y., & Rachmawati, I. N. (2014). Qualitative research methodology in nursing research. Rajawali Press.
Alfulayw, K. H., Al-Otaibi, S. T., & Alqahtani, H. A. (2021). Factors associated with needlestick injuries among healthcare workers: Implications for prevention. BMC Health Services Research, 21(1), 1–8. https://doi.org/10.1186/s12913-021-07110-y PMID: 34627244
Alves, M. J., Pina, D., Puente-López, E., Luna-Maldonado, A., Ruiz-Cabello, A. L., Magalhães, T., Pina-López, Y., Ruiz-Hernández, J. A., & Jarreta, B. M. (2021). Tough love lessons: Lateral violence among hospital nurses. International Journal of Environmental Research and Public Health, 18(17), 1–17. https://doi.org/10.3390/ijerph18179183
An, S., Ham, S., Lee, W., Choi, W., & Kang, S. (2020). Occupational diseases among health workers. Journal of Korean Society of Occupational and Environmental Hygiene, 30(4), 353–363. https://doi.org/10.15269/JKSOEH.2020.30.4.353
Badan Pusat Statistik. (2024). Badan Pusat Statistik Provinsi Kalimantan Utara. Retrieved from https://kaltara.bps.go.id/pressrelease/2021/01/21/287/jumlah-penduduk-provinsi-kalimantan-utara-hasil-sensus-penduduk-2020--september-2020--berjumlah-701-814-jiwa.html
Hidayati, H. B. (2022). Low back pain. Airlangga University Press. Retrieved from https://www.google.co.id/books/edition/Nyeri_Punggung_Bawah/rw1pEAAAQBAJ?hl=en&gbpv=1
Indragiri, S., & Yuttya, T. (2020). Occupational health and safety risk management using Hazard Identification Risk Assessment and Risk Control (HIRARC). Jurnal Kesehatan, 9(1), 1080–1094. https://doi.org/10.38165/jk.v9i1.77
Keefe, A. R., Demers, P. A., Neis, B., Arrandale, V. H., Davies, H. W., Gao, Z., Hedges, K., Holness, D. L., Koehoorn, M., Stock, S. R., & Bornstein, S. (2020). A scoping review to identify strategies that work to prevent four important occupational diseases. American Journal of Industrial Medicine, 63(6), 490–516. https://doi.org/10.1002/ajim.23107
Ma, H., Huang, S. Q., We, B., & Zhong, Y. (2022). Compassion fatigue, burnout, compassion satisfaction, and depression among emergency department physicians and nurses: A cross-sectional study. BMJ Open, 12(4), 1–6. https://doi.org/10.1136/bmjopen-2021-055941
Okpala, P. (2020). Nurses’ perspectives on the impact of management approaches on the blame culture in healthcare organizations. International Journal of Healthcare Management, 13(1), 199–205. https://doi.org/10.1080/20479700.2018.1492771
Polit, D. F., & Beck, C. T. (2017). Nursing research: Generating and assessing evidence for nursing practice (10th ed.). Wolters Kluwer Health.
Prajwal, M. S., Kundury, K. K., & Sujay, M. J. (2020). Assessing awareness of occupational safety and health hazards among nursing staff of a teaching hospital. Journal of Family Medicine and Primary Care, 9(12), 5961–590. https://doi.org/10.4103/jfmpc.jfmpc
Rai, R., El-Zaemey, S., Dorji, N., Rai, B. D., & Fritschi, L. (2021). Exposure to occupational hazards among healthcare workers in low-and middle-income countries: A scoping review. International Journal of Environmental Research and Public Health, 18(5), 1–41. https://doi.org/10.3390/ijerph18052603
Rasool, S. F., Wang, M., Zhang, Y., & Samma, M. (2020). Sustainable work performance: The roles of workplace violence and occupational stress. International Journal of Environmental Research and Public Health, 17(3). https://doi.org/10.3390/ijerph17030912
Restuputri, D. P., Rifdah, N. T., & Masudin, I. (2024). Building a work safety climate: Theory, strategy, and practice. UMMPress.
Risanti, R. D., Purwanti, E., & Novyriana, E. (2021). Factors related to nurses' compliance with implementing the Surgical Safety Checklist in the Central Surgical Installation. Jurnal Berita Ilmu Keperawatan, 14(2), 80–91.
RSUP dr. Soeradji Tirtonegoro Klaten. (2022). Low back pain. In Kemenkes Direktorat Jendral Pelayanan Kesehatan. Retrieved from https://yankes.kemkes.go.id/view_artikel/1149/intoksikasi-alkohol
Saleh, M., Wali, M., Hassan, O., Bayomy, H., & Nabil, N. (2020). Occupational hazards risk assessment of nurses working in operating rooms. Egyptian Journal of Occupational Medicine, 43(3), 793–808. https://doi.org/10.21608/ejom.2020.118360
Shan, G., Wang, S., Wang, W., Guo, S., & Li, Y. (2021). Presenteeism in nurses: Prevalence, consequences, and causes from the perspectives of nurses and chief nurses. Frontiers in Psychiatry, 11(January), 1–10. https://doi.org/10.3389/fpsyt.2020.584040
Sofiantika, D., & Susilo, R. (2020). The relationship between workload and work environment with occupational accidents in nurses in inpatient wards at RSUD Banyumas. Jurnal Keperawatan Muhammadiyah, September, 249–253. https://doi.org/10.30651/jkm.v0i0.5436
Suhaya, I., & Sari, H. (2019). The stress level of nurses in caring for patients with infectious diseases at the Dr. Zainole Abidin Banda Aceh Regional General Hospital. Jim Fkep, IV(1), 102–106. Retrieved from https://jim.usk.ac.id/FKep/article/view/11835
Yulis, R. (2020). The experience of head nurses identifying occupational diseases and accidents: A qualitative study. Jurnal Ilmiah Perawat Manado, 08(01), 108–126. https://doi.org/10.47718/jpd.v8i01.1011
Yulis, R., Pawenrusi, E. P., & Amalia, N. (2023). Violent behavior toward nurses in psychiatric wards. Kesehatan, 16(1), 19–27. https://doi.org/10.24252/kesehatan.v16i1.37340
Submitted
Accepted
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Rahma Yulis, Gusni Fitri, Fitriani Fitriani

This work is licensed under a Creative Commons Attribution 4.0 International License.


















