Predictors of Sleep Quality Among Type 2 Diabetes Mellitus Patients
DOI:
https://doi.org/10.23917/bik.v17i1.3529Keywords:
perceived stress scale, sleep quality, predictor, Type 2 Diabetes Mellitus PatientsAbstract
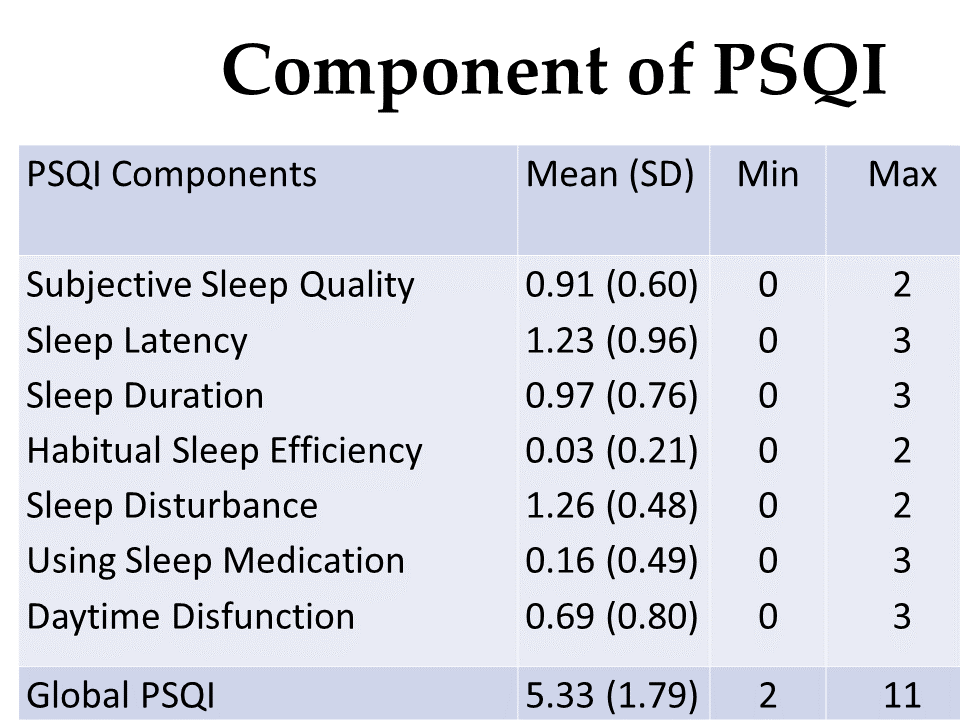
One of the health problems experienced by patients with type 2 diabetes mellitus is poor sleep quality. Poor sleep quality is an important factor in poor blood sugar regulation. This study aims to determine the predictors of sleep quality in patients with type 2 diabetes mellitus at a private hospital in Yogyakarta. This research was conducted using a cross sectional approach on 150 type 2 diabetes mellitus patients who were recruited at the Endocrine Clinic at a private hospital in Yogyakarta. The questionnaires used in this research were demographic data questionnaires, Perceived Stress Scale (PSS-10), Pittsburgh Sleep Quality Index (PSQI). Data analysis was carried out using Multiple hierarchical linear regression. The research results show that the average stress score of respondents in this study was 16.13 (SD = 4.59), which is in the medium category. Global PSQI showed that respondents experienced poor sleep quality (mean = 5.33, SD = 1.79). The Perceived Stress Scale score contributed 23.6% to the sleep quality score. The higher the respondent's stress level, the lower the respondent's sleep quality. Nurses can develop interventions to improve the sleep quality of type 2 diabetes mellitus patients.
Downloads
References
Abdu, Y., Naja, S., Izham, M., Ibrahim, M., Abdou, M., Ahmed, R., … Bougmiza, I. (2023). Sleep Quality Among People with Type 2 Diabetes Mellitus During COVID-19 Pandemic : Evidence from Qatar’s National Diabetes Center. Diabetes, Metabolic Syndrome and Obesity, (May), 2803–2812. https://doi.org/10.2147/DMSO.S421878 DOI: https://doi.org/10.2147/DMSO.S421878
Arora, T., Chen, M. Z., Omar, O. M., Cooper, A. R., Andrews, R. C., & Taheri, S. (2016). An investigation of the associations among sleep duration and quality, body mass index, and insulin resistance in newly diagnosed type 2 diabetes mellitus patients. 3–11. https://doi.org/10.1177/2042018815616549 DOI: https://doi.org/10.1177/2042018815616549
Barakat, S., Abujbara, M., & Banimustafa, R. (2019). Sleep Quality in Patients With Type 2 Diabetes Mellitus. Journal of Clinical Medicine Research, 11(4), 261–266. https://doi.org/10.14740/jocmr2947w DOI: https://doi.org/10.14740/jocmr2947w
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index : A New Instrument Psychiatric Practice and Research. Psychiatry Research, 28. https://doi.org/https://doi.org/10.1016/0165-1781(89)90047-4. https://doi.org/10.1016/0165-1781(89)90047-4 DOI: https://doi.org/10.1016/0165-1781(89)90047-4
Cohen, S. (1988). Perceived stress in a probability sample of the United States. In S. Spacapan, & S. Oskamp (Eds.). The Social Psychology of Health, 31–67.
Feldman, E. L., Callaghan, B. C., Pop-busui, R., Zochodne, D. W., Wright, D. E., Bennett, D. L., … Viswanathan, V. (2019). Diabetic neuropathy. Nature Reviews Disease Primers, 5(41). https://doi.org/10.1038/s41572-019-0092-1 DOI: https://doi.org/10.1038/s41572-019-0092-1
Fontela, P. C., & Berlezi, E. M. (2015). Sleep Respiratory Disorders and Clinical Pro fi le in Patients with Type 2 Diabetes Mellitus. International Archives of Otorhinolaryngology., 19. https://doi.org/10.1055/s-0034-1395998 DOI: https://doi.org/10.1055/s-0034-1395998
Gupta, S., & Bansal, S. (2020). Does a rise in BMI cause an increased risk of diabetes ?: Evidence from India. Plos One, 15(4), 1–20. https://doi.org/10.1371/journal.pone.0229716 DOI: https://doi.org/10.1371/journal.pone.0229716
Haveleia, A., & Gayatri, D. (2019). Sleep quality and the affecting factors in patients with diabetic ulcer ଝ. Enfermería Clínica, 29, 70–75. https://doi.org/10.1016/j.enfcli.2019.04.011. IDF. (2021). IDF Diabetes Atlas. Retrieved from https://diabetesatlas.org/atlas/tenth-edition/ DOI: https://doi.org/10.1016/j.enfcli.2019.04.011
Joensen, L. E., Madsen, K. P., Rod, N. H., Willaing, I., Holm, L., Nielsen, K. A., … Petersen, A. A. (2020). Research : Educational and Psychological Aspects Diabetes and COVID-19 : psychosocial consequences of the COVID-19 pandemic in people with diabetes in Denmark — what characterizes people with high levels of COVID-19-related worries ? Diabetic Medicine, 1146–1154. https://doi.org/10.1111/dme.14319 DOI: https://doi.org/10.1111/dme.14319
Kang, H. (2021). Sample size determination and power analysis using the G * Power software. Journal of Educational Evaluation for Health Professions, 18, 1–12. https://doi.org/10.3352/jeehp.2021.18.17 DOI: https://doi.org/10.3352/jeehp.2021.18.17
Kautzky-Willer, A., Harreiter, J., & Pacini, G. (2016). Sex and Gender Differences in Risk, Pathophysiology and Complications of Type 2 Diabetes Mellitus. Endocrine Review, 37(3), 278–316. https://doi.org/10.1210/er.2015-1137 DOI: https://doi.org/10.1210/er.2015-1137
Kelly, S. J., & Ismail, M. (2015). Stress and Type 2 Diabetes : A Review of How Stress Contributes to the Development of Type 2 Diabetes. The Annual Review OfPublic Health, 36, 441–462. https://doi.org/10.1146/annurev-publhealth-031914-122921 DOI: https://doi.org/10.1146/annurev-publhealth-031914-122921
Lou, P., Qin, Y., Zhang, P., Chen, P., Zhang, L., Chang, G., … Zhang, N. (2014). Association of sleep quality and quality of life in type 2 diabetes mellitus: A cross-sectional study in China. Diabetes Research and Clinical Practice. https://doi.org/10.1016/j.diabres.2014.09.060 DOI: https://doi.org/10.1016/j.diabres.2014.09.060
Merrill, R. M. (2022). Mental Health Conditions According to Stress and Sleep Disorders. International Journal of Environmental Research and Public Health, 19. https://doi.org/10.3390/ijerph19137957 DOI: https://doi.org/10.3390/ijerph19137957
Mohammed, S., Sokwalla, R., Joshi, M. D., Amayo, E. O., Acharya, K., Mecha, J. O., & Mutai, K. K. (2017). Quality of sleep and risk for obstructive sleep apnoea in ambulant individuals with type 2 diabetes mellitus at a tertiary referral hospital in Kenya : a cross-sectional , comparative study. 1–8. DOI: https://doi.org/10.1186/s12902-017-0158-6
Mordarska, K., & Godziejewska-zawada, M. (2017). Diabetes in the elderly. Przegląd Menopauzalny, 16(2), 38–43. https://doi.org/10.5114/pm.2017.68589 DOI: https://doi.org/10.5114/pm.2017.68589
Osonoi, Y., Mita, T., Osonoi, T., Saito, M., Tamasawa, A., Nakayama, S., … Watada, H. (2015). Poor sleep quality is associated with increased arterial stiffness in Japanese patients with type 2 diabetes mellitus. BMC Endocrine Disorders, 1–7. https://doi.org/10.1186/s12902-015-0026-1 DOI: https://doi.org/10.1186/s12902-015-0026-1
Prather, A. A., Bogdan, R., & Hariri, A. R. (2013). NIH Public Access. Psychosom Med, 75(4), 350–358. https://doi.org/10.1097/PSY.0b013e31828ef15b DOI: https://doi.org/10.1097/PSY.0b013e31828ef15b
Rautio, N., Varanka-ruuska, T., Vaaramo, E., & Ala-mursula, L. (2017). Accumulated exposure to unemployment is related to impaired glucose metabolism in middle-aged men : A follow-up of the Northern Finland Birth Cohort 1966. Primary Care Diabetes, 11(4), 365–372. https://doi.org/10.1016/j.pcd.2017.03.010 DOI: https://doi.org/10.1016/j.pcd.2017.03.010
Schäfer, T., & Schwarz, M. A. (2019). The Meaningfulness of Effect Sizes in Psychological Research : Differences Between Sub-Disciplines and the Impact of Potential Biases. The Journal Frontiers in Psychologyournal Frontiers in Psychology, 10(April), 1–13. https://doi.org/10.3389/fpsyg.2019.00813 DOI: https://doi.org/10.3389/fpsyg.2019.00813
Shibabaw, Y. Y., Dejenie, T. A., & Tesfa, K. H. (2023). Glycemic control and its association with sleep quality and duration among type 2 diabetic patients. Metabolism Open, 18(March), 100246. https://doi.org/10.1016/j.metop.2023.100246' DOI: https://doi.org/10.1016/j.metop.2023.100246
Steele, C. J., Schöttker, B., Marshall, A. H., Kouvonen, A., Doherty, M. G. O., Mons, U., … Kee, F. (2017). Education achievement and type 2 diabetes — what mediates the relationship in older adults ? Data from the ESTHER study : a population-based cohort study. 4–6. https://doi.org/10.1136/bmjopen-2016-013569 DOI: https://doi.org/10.1136/bmjopen-2016-013569
Westman, E. C. (2021). Type 2 Diabetes Mellitus : A Pathophysiologic Perspective. 8(August), 1–5. https://doi.org/10.3389/fnut.2021.707371 DOI: https://doi.org/10.3389/fnut.2021.707371
Yunzhao, T., Lingling, M., Daiqing, L., Min, Y., Yanjuan, Z., Chenguang, L., … Changlin, N. (2014). Interaction of sleep quality and sleep duration on glycemic control in patients with type 2 diabetes mellitus. Chinese Medical Journal, 127(20). Retrieved from https://pubmed.ncbi.nlm.nih.gov/25316226/https://doi.org/10.3760/cma.j.issn.0366-6999.20141512 DOI: https://doi.org/10.3760/cma.j.issn.0366-6999.20141512
Zhao, F. fang, Suhonen, R., Katajisto, J., & Leino-Kilp, H. (2018). The association of diabetes-related self-care activities with perceived stress , anxiety , and fatigue : a cross-sectional study. Patient Prefer Adherence, 12, 1677–1686. https://doi.org/10.2147/PPA.S169826 DOI: https://doi.org/10.2147/PPA.S169826
Zhao, X., Lan, M., Li, H., & Yang, J. (2020). Perceived stress and sleep quality among the non-diseased general public in China during the 2019 coronavirus disease : a moderated mediation model. Sleep Medicine, (January). https://doi.org/10.1016/j.sleep.2020.05.021 DOI: https://doi.org/10.1016/j.sleep.2020.05.021
Submitted
Accepted
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Dita Hanna Febriani

This work is licensed under a Creative Commons Attribution 4.0 International License.


















