Sleep And Hba1c In Adult Patients With Type 2 Diabetes Mellitus
DOI:
https://doi.org/10.23917/bik.v16i2.1764Keywords:
Hemoglobin A1c, Quality of Sleep, Type 2 Diabetes MellitusAbstract
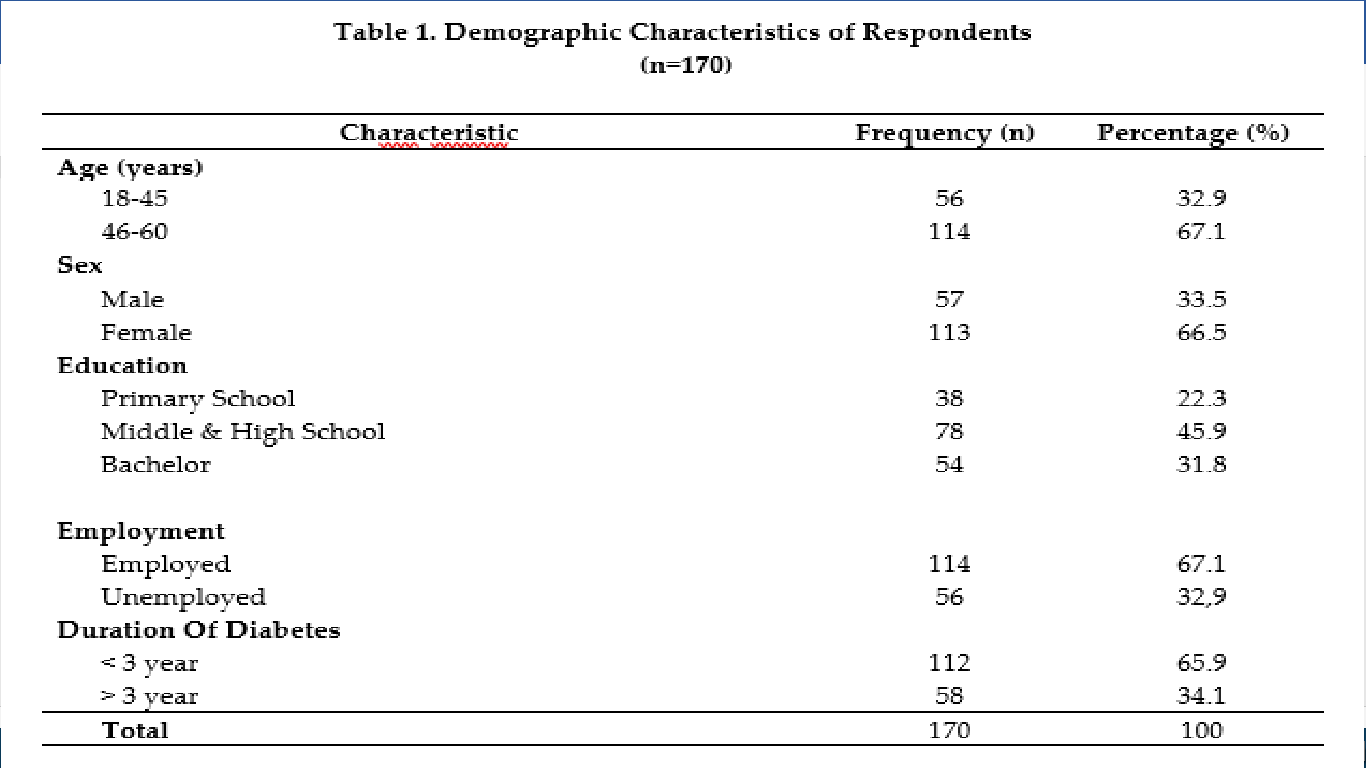
Sleep is one of the essential factors in life and affects glucose metabolism, so it is crucial for diabetic patients to have good quality sleep to control their diabetes. The study aimed to analyze the relationship between sleep quality and HbA1c levels in adult patients with type 2 diabetes mellitus. This study was conducted with a cross-sectional study approach with a sample of 170 respondents with convenience sampling from a hospital in Banda Aceh. Sleep quality data was measured by the Pittsburgh Sleep Quality Index (PSQI), and HbA1c levels were obtained from the results of respondents' HbA1c examinations in the last three months analyzed through chi-square. The results showed a significant relationship between sleep quality and respondents' HbA1c levels (p = 0.008), where respondents (64.1%) with poor sleep quality had an eight times the risk of having uncontrolled HbA1c levels compared to respondents with good sleep quality. Education on the importance of sleep health in patients regularly should be carried out in groups by health services to motivate T2DM patients to enjoy adequate sleep and improve their glycemic control through learning media that interest patients
Downloads
References
American Diabetes Association. (2017). Standards of medical care in diabetes-2017. Diabetes Care, 40(Suppl 1). https://doi.org/10.1111/1753-0407.12424
American Diabetes Association Professional Practice Committee. (2022). Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes—2022. Diabetes Care, 45 (Suppl.(January), S60–S82. https://doi.org/10.2337/dc22-S005
Azharuddin, M., Kapur, P., Adil, M., Ghosh, P., & Sharma, M. (2020). The impact of sleep duration and sleep quality on glycaemic control in Asian population with type 2 diabetes mellitus: A systematic literature review and meta-analysis of observational studies. Clinical Epidemiology and Global Health, 8(3), 967–975. https://doi.org/10.1016/j.cegh.2020.03.006
Azizah, U. N., Wurjanto, M. A., Kusariana, N., & Susanto, H. S. (2022). Hubungan Kualitas Tidur dengan Kontrol Glikemik pada Penderita Diabetes Melitus : Systematic Review. Jurnal Epidemiologi Kesehatan Komunitas, 7(1), 411–422. https://doi.org/10.14710/jekk.v7i1.13310
Barakat, S., Abujbara, M., Banimustafa, R., Batieha, A., & Ajlouni, K. (2019). Sleep Quality in Patients With Type 2 Diabetes Mellitus. Journal of Clinical Medicine Research, 11(4), 261–266. https://doi.org/10.14740/jocmr2947w
Bellon, F., Mora-Noya, V., Pastells-Peiró, R., Abad-Corpa, E., Gea-Sánchez, M., & Moreno-Casbas, T. (2021). The efficacy of nursing interventions on sleep quality in hospitalized patients: A systematic review of randomized controlled trials. International Journal of Nursing Studies, 115, 103855. https://doi.org/10.1016/j.ijnurstu.2020.103855
Buysse, D. J., Hall, M. L., Strollo, P. J., Kamarck, T. W., Owens, J., Lee, L., Reis, S. E., & Matthews, K. A. (2008). Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/polysomnographic measures in a community sample. Journal of Clinical Sleep Medicine, 4(6), 563–571. https://doi.org/10.5664/jcsm.27351
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Chang, C. J., Pei, D., Wu, C. C., Palmer, M. H., Su, C. C., Kuo, S. F., & Liao, Y. M. (2017). Correlates of Nocturia and Relationships of Nocturia With Sleep Quality and Glycemic Control in Women With Type 2 Diabetes. Journal of Nursing Scholarship, 49(4), 400–410. https://doi.org/10.1111/jnu.12302
Chasens, E. R., Korytkowski, M., Sereika, S. M., & Burke, L. E. (2013). Effect of Poor Sleep Quality and Excessive Daytime Sleepiness on Factors Associated with Diabetes Self-Management. Diabetes Educator, 39(1), 74–82. https://doi.org/10.1177/0145721712467683.Effect
Grossman, S., & Porth, C. M. (2014). Porth’s Pathophysiology: Concepts of Altered Health States-9th edition. (Ninth edit). Lippincott Williams & Wilkins.
Gupta, S., & Wang, Z. (2016). Predictors of sleep disorders among patients with type 2 diabetes mellitus. Diabetes and Metabolic Syndrome: Clinical Research and Reviews, 10(4), 213–220. https://doi.org/10.1016/j.dsx.2016.06.009
Hogenkamp, P. S., Nilsson, E., Nilsson, V. C., Chapman, C. D., Vogel, H., Lundberg, L. S., Zarei, S., Cedernaes, J., Rångtell, F. H., Broman, J. E., Dickson, S. L., Brunstrom, J. M., Benedict, C., & Schiöth, H. B. (2013). Acute sleep deprivation increases portion size and affects food choice in young men. Psychoneuroendocrinology, 38(9), 1668–1674. https://doi.org/10.1016/j.psyneuen.2013.01.012
International Diabetes Federation. (2021). IDF Diabetes Atlas 10th edition. In IDF. https://doi.org/10.1016/j.diabres.2013.10.013
Khalil, M., Power, N., Graham, E., Deschênes, S. S., & Schmitz, N. (2020). The association between sleep and diabetes outcomes – A systematic review. Diabetes Research and Clinical Practice, 161, 1–12. https://doi.org/10.1016/j.diabres.2020.108035
Khandelwal, D., Dutta, D., Chittawar, S., & Kalra, S. (2017). Sleep disorders in type 2 diabetes. Indian Journal of Endocrinology and Metabolism, 21(5), 758–761. https://doi.org/10.4103/ijem.IJEM_156_17
Lee, S. W. H., Ng, K. Y., & Chin, W. K. (2017a). The impact of sleep amount and sleep quality on glycemic control in type 2 diabetes: A systematic review and meta-analysis. Sleep Medicine Reviews, 31, 91–101. https://doi.org/10.1016/j.smrv.2016.02.001
Lee, S. W. H., Ng, K. Y., & Chin, W. K. (2017b). The impact of sleep amount and sleep quality on glycemic control in type 2 diabetes: A systematic review and meta-analysis. Sleep Medicine Reviews, 31, 91–101. https://doi.org/10.1016/j.smrv.2016.02.001
Lim, W. Y., Ma, S., Heng, D., Tai, E. S., Khoo, C. M., & Loh, T. P. (2018). Screening for diabetes with HbA1c: Test performance of HbA1c compared to fasting plasma glucose among Chinese, Malay and Indian community residents in Singapore. Scientific Reports, 8(1), 1–9. https://doi.org/10.1038/s41598-018-29998-z
Luyster, F. S., & Dunbar-Jacob, J. (2011). Sleep quality and quality of life in adults with type 2 diabetes. Diabetes Educator, 37(3), 347–355. https://doi.org/10.1177/0145721711400663
Menteri Kesehatan Republik Indonesia. (2016). Peraturan Menteri Kesehatan Republik Indonesia Nomor 25 Tahun 2016 Tentang Rencana Aksi Nasional Kesehatan Lanjut Usia Tahun 2016-2019. In http://hukor.kemkes.go.id/uploads/produk_hukum/PMK_No._25_ttg_Rencana_Aksi_Nasional_Kesehatan_Lanjut_Usia_Tahun_2016-2019_.pdf.
Obayashi, K., Saeki, K., Iwamoto, J., Okamoto, N., Tomioka, K., Nezu, S., Ikada, Y., & Kurumatani, N. (2013). Exposure to Light at Night, Nocturnal Urinary Melatonin Excretion, and Obesity/Dyslipidemia in the Elderly: A Cross-Sectional Analysis of the HEIJO-KYO Study. Journal of Clinical Endocrinology & Metabolism, 98(1), 337–344. https://doi.org/10.1210/jc.2012–2874
Ohkuma, T., Fujii, H., Iwase, M., Ogata-Kaizu, S., Ide, H., Kikuchi, Y., Idewaki, Y., Jodai, T., Hirakawa, Y., Nakamura, U., & Kitazono, T. (2014). U-shaped association of sleep duration with metabolic syndrome and insulin resistance in patients with type 2 diabetes: The Fukuoka Diabetes Registry. Metabolism: Clinical and Experimental, 63(4), 484–491. https://doi.org/10.1016/j.metabol.2013.12.001
Pejovic, S., Vgontzas, A. N., Basta, M., Tsaoussoglou, M., Zoumakis, E., Vgontzas, A., Bixler, E. O., & Chrousos, G. P. (2010). Leptin and Hunger Levels in Young Healthy Adults After One Night of Sleep Loss. J Sleep Res, 19(4), 552–558. https://doi.org/10.1111/j.1365-2869.2010.00844.x.Leptin
Rajendran, A., Parthsarathy, S., Tamilselvan, B., Seshadri, K. G., & Shuaib, M. (2012). Prevalence and correlates of disordered sleep in southeast asian indians with type 2 diabetes. Diabetes and Metabolism Journal, 36(4), 314–315. https://doi.org/10.4093/dmj.2012.36.4.314
Resnick, H. E., Redline, S., Shahar, E., Gilpin, A., Newman, A., Walter, R., Ewy, G. a, Howard, B. V, & Punjabi, N. M. (2003). Findings from the Sleep Heart Health Study. Diabetes Care, 26(3), 702–709. http://care.diabetesjournals.org/content/26/3/702.short
Smyth, A., Jenkins, M., Dunham, M., Kutzer, Y., Taheri, S., & Whitehead, L. (2020). Systematic review of clinical practice guidelines to identify recommendations for sleep in type 2 diabetes mellitus management. Diabetes Research and Clinical Practice, 170, 108532. https://doi.org/10.1016/j.diabres.2020.108532
Soelistijo, S. A., Lindarto, D., Decroli, E., Permana, H., Sucipto, K. W., Kusnadi, Y., Budiman, Ikhsan, R., Sasiarini, L., & Sanusi, H. (2019). Pedoman Pengelolaan Dan Pencegahan Diabetes Melitus Tipe 2 Dewasa di Indonesia. In PB Perkumpulan Endokrinologi Indonesia (Perkeni).
Sondrup, N., Termannsen, A. D., Eriksen, J. N., Hjorth, M. F., Færch, K., Klingenberg, L., & Quist, J. S. (2022). Effects of sleep manipulation on markers of insulin sensitivity: A systematic review and meta-analysis of randomized controlled trials. Sleep Medicine Reviews, 62, 101594. https://doi.org/10.1016/j.smrv.2022.101594
Surani, S. (2015). Effect of diabetes mellitus on sleep quality. World Journal of Diabetes, 6(6), 868. https://doi.org/10.4239/wjd.v6.i6.868
Taheri, S., Lin, L., Austin, D., Young, T., & Mignot, E. (2004). Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Medicine, 1(3), 210–217. https://doi.org/10.1371/journal.pmed.0010062
Tan, X., & Benedict, C. (2020). Sleep characteristics and HbA1c in patients with type 2 diabetes on glucose-lowering medication. BMJ Open Diabetes Research and Care, 8(1), 2–8. https://doi.org/10.1136/bmjdrc-2020-001702
Tan, X., van Egmond, L., Chapman, C. D., Cedernaes, J., & Benedict, C. (2018). Aiding sleep in type 2 diabetes: therapeutic considerations. The Lancet Diabetes and Endocrinology, 6(1), 60–68. https://doi.org/10.1016/S2213-8587(17)30233-4
Tsai, Y. W., Kann, N. H., Tung, T. H., Chao, Y. J., Lin, C. J., Chang, K. C., Chang, S. S., & Chen, J. Y. (2012). Impact of subjective sleep quality on glycemic control in type 2 diabetes mellitus. Family Practice, 29(1), 30–35. https://doi.org/10.1093/fampra/cmr041
Zahra, A. N., & Farida, M. E. (2020). Hubungan Kadar HbA1c dan Kualitas Tidur pada Pasien Diabetes Melitus Tipe 2. Jurnal Persatuan Perawat Nasional Indonesia (JPPNI), 3(3), 189. https://doi.org/10.32419/jppni.v3i3.170
Zhu, B. Q., Li, X. M., Wang, D., & Yu, X. F. (2014). Sleep quality and its impact on glycaemic control in patients with type 2 diabetes mellitus. International Journal of Nursing Sciences, 1(3), 260–265. https://doi.org/10.1016/j.ijnss.2014.05.020
Zhu, B., Vincent, C., Kapella, M. C., Quinn, L., Collins, E. G., Ruggiero, L., Park, C., & Fritschi, C. (2018). Sleep disturbance in people with diabetes: A concept analysis. Journal of Clinical Nursing, 27(1–2), 1–19. https://doi.org/10.1111/jocn.14010
Downloads
Submitted
Accepted
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Rizki Andriani, Orita Satria, Nurhadia Nurhadia, Crasdian Afri Yudi

This work is licensed under a Creative Commons Attribution 4.0 International License.