An Analysis of Community Satisfaction Index on Health Service Quality: CFA and Gap Analysis
DOI:
https://doi.org/10.23917/bik.v16i2.2369Keywords:
Confirmatory Factor Analysis, Community Satisfaction Index, Quality of Service, Performance, ExpectationsAbstract
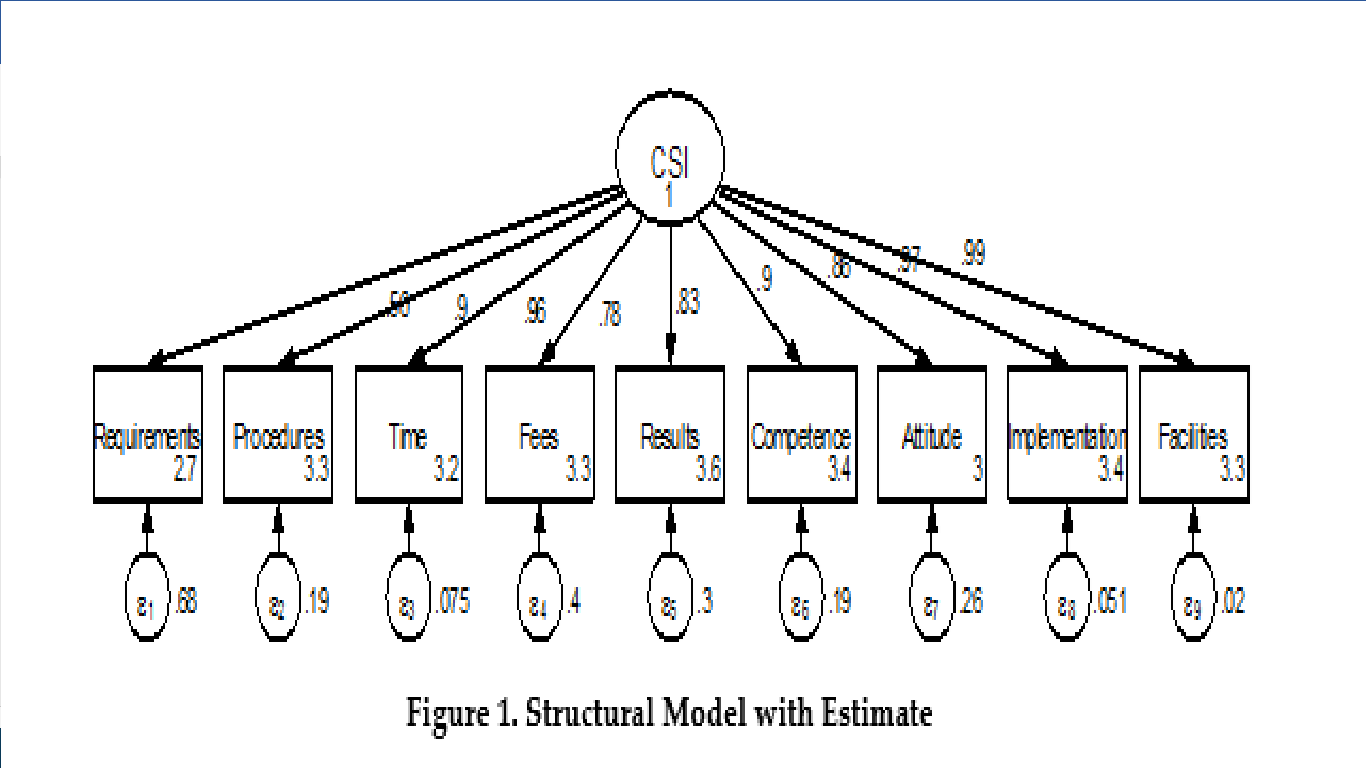
The Community Satisfaction Index is the focus of attention because it is a reference in evaluating health service policies on the quality of hospital services. Service quality is a determinant factor of patient safety to reduce the incidence of mortality in hospitals. Crossectional is the research design used. The study was conducted from April to June 2023, the population is all patients in the hospital in 2023, and Simple random side as a sampling technique of 136 research subjects. The research variables are performance, expectations, and the Community Satisfaction Index which consists of nine elements, namely requirements; systems, mechanisms, and procedures; turnaround time; cost; product specification type of service; competence of the executor; executor behavior; handling of complaints, suggestions, and inputs. Data collection using questionnaires that have previously been tested for confirmatory factor analysis. Test questionnaires and analyze research results with gap analysis using Wilcoxon in the STATA program. The test results of confirmatory factor analysis showed that RMSEA values = 0.04, CFI = 0.99, χ2 / df = 1.05, and TLI = 0.99 showed that the model met goodness-of-fit. The gap analysis shows that in the 9 elements of the Community Satisfaction Index, 2 elements are not different, namely the competence of the implementer (z = -1.570, p = 0.116) and the behavior of the implementer (z = -1.414, p = 0.157). It is hoped that the results of the research can be used as material for the evaluation of hospital policies.
Downloads
References
Ai, Y., Rahman, M. K., Newaz, M. S., Gazi, M. A. I., Rahaman, M. A., Mamun, A. Al, & Chen, X. (2022). Determinants of patients’ satisfaction and trust toward healthcare service environment in general practice clinics. Frontiers in Psychology, 13. https://doi.org/10.3389/fpsyg.2022.856750
Arsita, R., & Idris, H. (2019). the Relationship of Hospital Cost, Service Quality and Patient Satisfaction. Jurnal Ilmu Kesehatan Masyarakat, 10(2), 132–138. https://doi.org/10.26553/jikm.2019.10.2.132-138
Asamrew, N., Endris, A. A., & Tadesse, M. (2020). Level of Patient Satisfaction with Inpatient Services and Its Determinants: A Study of a Specialized Hospital in Ethiopia. Journal of Environmental and Public Health, 2020. https://doi.org/10.1155/2020/2473469
Chen, W., Shi, Y., Fan, L., Huang, L., & Gao, J. (2021). Influencing factors of public satisfaction with covid-19 prevention services based on structural equation modeling (Sem): A study of Nanjing, China. International Journal of Environmental Research and Public Health, 18(24). https://doi.org/10.3390/ijerph182413281
Endeshaw, B. (2021). Healthcare service quality-measurement models: a review. Journal of Health Research, 35(2), 106–117. https://doi.org/10.1108/JHR-07-2019-0152
Hoseini-Esfidarjani, S. S., Negarandeh, R., Delavar, F., & Janani, L. (2021). Psychometric evaluation of the perceived access to health care questionnaire. BMC Health Services Research, 21(1), 1–10. https://doi.org/10.1186/s12913-021-06655-2
Izadi, A., Jahani, Y., Rafiei, S., Masoud, A., & Vali, L. (2017). Evaluating health service quality: using importance performance analysis. International Journal of Health Care Quality Assurance, 30(7), 656–663. https://doi.org/10.1108/IJHCQA-02-2017-0030
Karaca, A., & Durna, Z. (2019). Patient satisfaction with the quality of nursing care. Nursing Open, 6(2), 535–545. https://doi.org/10.1002/nop2.237
Ke, L., Chen, J., Jia, J., Ke, P., Chen, X., Mao, Z., & Liu, B. (2020). Outpatients’ satisfaction in the context of 10 years of health-care reform: A cross-sectional study of tertiary hospitals in shiyan, China. Patient Preference and Adherence, 14, 191–202. https://doi.org/10.2147/PPA.S233472
Kemenkes. (2020). Permenkes RI Nomor 21 Tahun 2020. Kementerian Kesehatan RI, 9(May), 6. https://www.slideshare.net/maryamkazemi3/stability-of-colloids%0Ahttps://barnard.edu/sites/default/files/inline/student_user_guide_for_spss.pdf%0Ahttp://www.ibm.com/support%0Ahttp://www.spss.com/sites/dm-book/legacy/ProgDataMgmt_SPSS17.pdf%0Ahttps://www.n
Kementrian Kesehatan RI. (2009). UU no. 44 Tahun 2009 Tentang RS. Undang-Undang Republik Indonesia, 1, 41. https://peraturan.go.id/common/dokumen/ln/2009/uu0442009.pdf
Kruk, M. E., Gage, A. D., Arsenault, C., Jordan, K., Leslie, H. H., Roder-DeWan, S., Adeyi, O., Barker, P., Daelmans, B., Doubova, S. V., English, M., Elorrio, E. G., Guanais, F., Gureje, O., Hirschhorn, L. R., Jiang, L., Kelley, E., Lemango, E. T., Liljestrand, J., … Pate, M. (2018). High-quality health systems in the Sustainable Development Goals era: time for a revolution. The Lancet Global Health, 6(11), e1196–e1252. https://doi.org/10.1016/S2214-109X(18)30386-3
Liu, S., Li, G., Liu, N., & Hongwei, W. (2021). The Impact of Patient Satisfaction on Patient Loyalty with the Mediating Effect of Patient Trust. Inquiry (United States), 58. https://doi.org/10.1177/00469580211007221
Mahendradhata, Y., Trisnantoro, L., Listyadewi, S., Soewondo, P., MArthias, T., Harimurti, P., & Prawira, J. (2017). The Republic of Indonesia Health System Review (Vol. 7, Issue 1).
Manzoor F, Wei L, Hussain A, Asif M, & Shah S. (2019). Patient satisfaction with health care services; an application of physician’s behavior as a moderator. International Journal of Environmental Research and Public Health [revista en Internet] 2019 [acceso 20 de octubre de 2022]; 16(18): 1-16. 1–16.
Mosadeghrad, A. M. (2014). Factors influencing healthcare service quality. International Journal of Health Policy and Management, 3(2), 77–89. https://doi.org/10.15171/ijhpm.2014.65
Musriha, S. R., & Hartatiek, W. (2021). Analysis of Community Satisfaction Index on Public Services in Industrial Revolution 4.0. PalArch’s Journal of Archaeology of …, 18(4), 1457–1472. https://archives.palarch.nl/index.php/jae/article/view/6504%0Ahttps://archives.palarch.nl/index.php/jae/article/download/6504/6338
Mutiarasari, D., Demak, I. P. K., Bangkele, E. Y., Nur, R., & Setyawati, T. (2021). Patient satisfaction: Public vs. private hospital in Central Sulawesi, Indonesia. Gaceta Sanitaria, 35(December), S186–S190. https://doi.org/10.1016/j.gaceta.2021.07.012
Osta Nababan, B., Nugroho, A., & Riadi, S. (2021). Analysis of Community Satisfaction with Public Services in The Bojong Gede District Office, Bogor Regency. Majalah Ilmiah Bijak, 18(3), 31–41. https://doi.org/10.31334/bijak.v19i1.1960
PermenPanRB. (2017). Cell density-dependent stimulation of glutamine synthetase activity in cultured mouse teratoma cells. In Peraturan Menteri Pendayaguaan Aparatur Negara dan Reformasi Birokrasi Republik Indonesia Nomor 14 Tahun 2017. https://doi.org/10.1016/0014-4827(75)90518-2
Prakoeswa, C. R. S., Hidayah, N., Dewi, A., Purnamasari, I., Adriansyah, A. A., & Yaqub, A. M. (2022). Patient Satisfaction, Perception-Expectation Gap, and Costumer Satisfaction Index in Annual Survey 2021 at Dr. Soetomo General Academic Hospital. Folia Medica Indonesiana, 58(2), 178–186. https://doi.org/10.20473/fmi.v58i2.34550
Prasaja, H. sukes, Setiyadi, N. A., & Kurniawan, A. (2014). Analisis sistem informasi registrasi pasien di rumah sakit umum asy-syifa sambi boyolali artikel publikasi ilmiah. Jurnal Teknik Informatika Dan Sistem Informasi, 3(2), 24–69.
Rahmah, A. H., Dharmawan, R., & Rahardjo, S. S. (2018). Socioeconomic, Environmental, and Behavioral Determinants of Leprosy in Kediri, East Java. Journal of Epidemiology and Public Health, 03(02), 253–262. https://doi.org/10.26911/jepublichealth.2018.03.02.05
Rohmawati, D., Setiyadi, N. A., & Werdani, K. E. (2014). Hubungan pengetahuan sikap dan sosial ekonomi dengan pemilihan jenis iuran keikutsertaan JKN Mandiri pada wilayah cakupan JKN tertinggi di Surakarta. 1–13. http://eprints.ums.ac.id/32416/
Sakawati, H., Agustina, N., & Sulmiah, S. (2021). The Influence of Service Quality on inpatients Satisfaction: Study at Bahagia Hospitals, Makassar City. Jurnal Office, 7(1), 21. https://doi.org/10.26858/jo.v7i1.19819
Setiyadi, N. A., & Hakam, F. (2015). Analysis of Health Information System in Muhammadiyah Medical Center (MMC) Muhammadiyah University of Surakarta. Jurnal IKESMA, 11(1), 1–14.
Shafiq, M., Naeem, M. A., Munawar, Z., & Fatima, I. (2017). Service quality assessment of hospitals in Asian context: An empirical evidence from Pakistan. Inquiry (United States), 54. https://doi.org/10.1177/0046958017714664
Sultan, N., Mahajan, R., Kumari, R., Langer, B., Guta, Rajiv, K., Mir, Menhak, T., Chowdhary, N., & Sultan, A. (2022). Patient satisfaction with hospital services in COVID‑19 era: A cross‑sectional study from outpatient department of a tertiary care hospital in Jammu, UT of J&K, India. Journal of Family Medicine and Primary Care, 11(10). https://doi.org/10.4103/jfmpc.jfmpc
Surury, I., Ali, L. H., & Prastiwi, N. D. (2022). Satisfaction of Non-Covid-19 Patients Under National Health Insurance (Jkn) in Changes in Health Services During the Covid-19 Pandemic and Associated Factors. Jurnal Ekonomi Kesehatan Indonesia, 7(1), 23. https://doi.org/10.7454/eki.v7i1.5442
Utami, S. P., Maarif, M. S., & Simanjuntak, M. (2022). Strategy for Increasing Consumer Satisfaction of Hospital Services Using Importance-Performance Analysis (IPA) Approach. Jurnal Aplikasi Bisnis Dan Manajemen, 8(2), 383–393. https://doi.org/10.17358/jabm.8.2.383
Verma, M., Rama, K., & Aggarwal, R. (2020). Assesment of Patients Statisfaction Visiting a Tertiary Health Care Institute in North India. Journal of Pharmacy and Bioallied Sciences, 12(3). https://doi.org/10.4103/jpbs.JPBS
WHO. (2018). Quality in primary health care. Preventive and Social Medicine, 54.
Woo, S., & Choi, M. (2021). Medical service quality, patient satisfaction and intent to revisit: Case study of public hub hospitals in the Republic of Korea. PLoS ONE, 16(6 June 2021), 1–14. https://doi.org/10.1371/journal.pone.0252241
Yakob, A., Kamariah, N., & Muttaqin. (2022). Jurnal midwifery. Jurnal Midwifery, 4(1). https://doi.org/10.24252/jmw.v4i1.28962
Downloads
Submitted
Accepted
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Lina Alfiyani, Noor Alis Setiyadi, Asmirati Yakob, Didik Mulyono, Rohmat Rohmat, Mohammad Fathur Rizqi

This work is licensed under a Creative Commons Attribution 4.0 International License.