The Issues Related to Children with Leukemia in Indonesia: An Integrative Review
DOI:
https://doi.org/10.23917/bik.v16i2.1871Keywords:
cancer, children, quality of life, Leukemia, IndonesiaAbstract
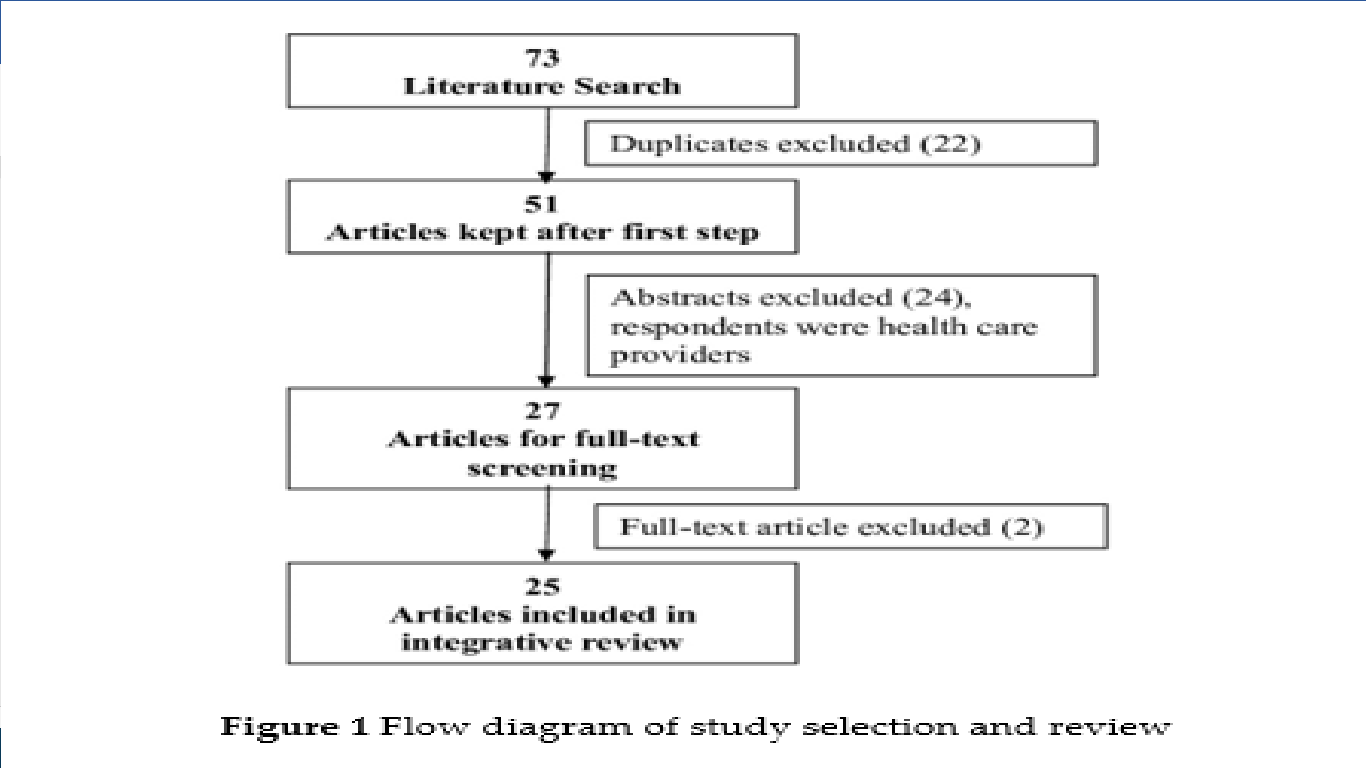
This integrative review, based on twenty-four studies from data resources, including Scopus, CINAHL, MEDLINE, PsycINFO, and Indonesia science and technology index (SINTA), was published from 2009 to 2019. The eligible studies were conducted in Indonesia, published in the English or Indonesian language, and reported the incident, survival rate, and physical or psychological effects of disease or chemotherapy. There were 23 quantitative studies and two qualitative studies. The theoretical or conceptual framework was not identified to guide and develop the studies. Most studies used retrospective and cross-sectional studies; the target population was acute lymphoblastic leukemia (ALL) and used small sample sizes for a cross-sectional study. The variables that were explored in the quantitative studies consisted of the incidence of leukemia, survival rate, abandonment of treatment, effects of disease or chemotherapy, quality of life (QOL), and others. The qualitative findings focused on the experience of being diagnosed with leukemia and its meaning in the adolescent context. The evidence from the studies showed that the incidence rate of all types of leukemia increases each year. The survival rate was lower than in other countries, with differences in numbers among hospitals. The effects of the disease and chemotherapy dominated the problem of children the low level of QOL. More research is necessary to explore the factors related to treatments' outcomes, particularly the aspects related to survival rate and QOL are using comprehensive data analysis, an appropriate theoretical framework to guide the study, more sample size, and involving multiple hospital settings.
Downloads
References
Adom, D., Hussain, E. K., & Joe, A. A. (2018). The theoretical and conceptual framework: Mandatory ingredients of a quality research. International Journal of Scientific Research, 7(1), 93–98. https://www.researchgate.net/publication/322204158%0ATHEORETICAL
Agnes, M., Widjajanto, H., Damayanti, W., Science, B., Children, K., Medicine, F., Gadjah, U., Rsup, M. /, & Sardjito, Y. (2019). The Incidence of Neutropenic Fever in Children's Acute Lymphoblastic Leukemia at RSUP Dr. Sardjito Yogyakarta The Incidence of Febrile Neutropenia in Childhood Acute Lymphoblastic Leukemia In Dr. Sardjito Hospital Yogyakarta. Sari Pediatrics, 20(6), 361–363. https://doi.org/10.14238/sp20.6.2019.360-5
Alfina, D., Widjajanto, P. H., & Patria, S. Y. (2011). The outcomes of childhood acute lymphoblastic leukemia with hyperleukocytosis. Paediatrica Indonesiana, 51(4), 186–191. https://doi.org/10.14238/pi58.4.2018.186-91
Anggraini, S. (2018). Hypnoparenting Effects Towards Fatigue As an Impact of Chemotherapy Among Pediatric Patients With Acute Lymphoblastic Leukemia. Indonesian Journal of Nursing, 21(2), 77–83. https://doi.org/10.7454/jki.v21i2.570
Arora, R. S., Pizer, B., & Eden, T. (2010). Understanding refusal and abandonment in the treatment of childhood cancer. Indian Pediatrics, 47(12), 1005–1010. https://doi.org/10.1007/s13312-010-0172-5
Bader, C., Cossin, S., Maillard, A., & Bénard, A. (2018). A new approach for sample size calculation in cost-effectiveness studies based on the value of information. BMC Medical Research Methodology, 18(1), 1–10. https://doi.org/10.1186/s12874-018-0571-1
Baguley, T. (2004). Understanding statistical power in the context of applied research. Applied Ergonomics, 35(2), 73–80. https://doi.org/10.1016/j.apergo.2004.01.002
Bidwell, S. S., Peterson, C. C., Demanelis, K., Zarins, K. R., Meza, R., Sriplung, H., Wiangnon, S., Chotsampancharoen, T., Chitapanarux, I., Pongnikorn, D., Daoprasert, K ., Suwanrungrung, K., Chansaard, W., & Rozek, L. S. (2019). Childhood cancer incidence and survival in Thailand: A comprehensive population-based registry analysis, 1990–2011. Pediatric Blood and Cancer, 66(1), 1–9. https://doi.org/10.1002/pbc.27428
Bonaventure, A., Harewood, R., Stiller, C. A., Gatta, G., Clavel, J., Stefan, D. C., Carreira, H., Spika, D., Marcos-Gragera, R., Peris-Bonet, R ., Piñeros, M., Sant, M., Kuehni, C. E., Murphy, M. F. G., Coleman, M. P., Allemani, C., Bouzbid, S., Hamdi-Chérif, M., Zaidi, Z., … Tanaka, L. F. (2017). Worldwide comparison of survival from childhood leukemia for 1995–2009, by subtype, age, and sex (CONCORD-2): a population-based study of individual data for 89 828 children from 198 registries in 53 countries. The Lancet Haematology, 4(5), e202–e217. https://doi.org/10.1016/S2352-3026(17)30052-2
Cai, J., Yu, J., Zhu, X., Hu, S., Zhu, Y., Jiang, H., Li, C., Fang, Y., Liang, C., Ju, X., Tian, X., Zhai, X., Hao, J., Hu, Q., Wang, N., Jiang, H., Sun, L., Li, C. K., Pan, K., … Tang, J. ( 2019). Treatment abandonment in childhood acute lymphoblastic leukemia in China: A retrospective cohort study of the Chinese Children's Cancer Group. Archives of Disease in Childhood, 104(6), 522–529. https://doi.org/10.1136/archdischild-2018-316181
Desouky, E. D. El, Noaman, M. K., Shalaby, L. M., & Shaaban, S. Y. (2017). Factors Affecting Quality of Life in Patients with Pediatric Leukemia during Induction Chemotherapy. The Egyptian Journal of Community Medicine, 35(4), 15–23. https://doi.org/10.21608/ejcm.2017.5037
Devi, K. S., & Allenidekania, A. (2019). The Relationship of Oral Care Practice at Home with Mucositis Incidence in Children with Acute Lymphoblastic Leukemia. Comprehensive Child and Adolescent Nursing, 42(sup1), 56–64. https://doi.org/10.1080/24694193.2019.1577926
Eche, I. J., & Aronowitz, T. (2018). Factors That Influence Parental Uncertainty and Health-Related Quality of Life in Children With Cancer: A Framework. Nursing Science Quarterly, 31(4), 362–368. https://doi.org/10.1177/0894318418792896
Eiser, C., Cotter, I., Oades, P., Seamark, D., & Smith, R. (1999). Health-related quality-of-life measures for children. International Journal of Cancer, 83(SUPPL. 12), 87–90. https://doi.org/10.1002/(sici)1097-0215(1999)83:12+<87::aid-ijc16>3.0.co;2-o
Eiser, C., & Morse, R. (2001). A review of measures of quality of life for children with chronic illness. Archives of Disease in Childhood, 84(3), 205–211. https://doi.org/10.1136/adc.84.3.205
Faber, J., & Fonseca, L. M. (2014). How sample size influences research outcomes. Dental Press Journal of Orthodontics, 19(4), 27–29. https://doi.org/10.1590/2176-9451.19.4.027-029.eboFadhilah, A., & Allenidekania, A. (2019). The Relationship between Activity Level and Fatigue in Indonesian Children with Acute Lymphocytic Leukemia in the Home Setting. Comprehensive Child and Adolescent Nursing, 42(sup1), 47–55. https://doi.org/10.1080/24694193.2019.1577925
Fardell, J. E., Vetsch, J., Trahair, T., Mateos, M. K., Grootenhuis, M. A., Touyz, L. M., Marshall, G. M., & Wakefield, C. E. (2017). Health-related quality of life of children on treatment for acute lymphoblastic leukemia: A systematic review. Pediatric Blood and Cancer, 64(9), 1–13. https://doi.org/10.1002/pbc.26489
Hapsari, M., Tamam, M., & Satrio, P. (2013). Risk factors for neutropenic fever in children with acute lymphoblastic leukemia. Sari Pediatrics, 15(1), 39–45. https://doi.org/10.14238/sp15.1.2013.39-45
Hazarika, M., Mishra, R., Saikia, B. J., Bhuyan, C., Nyuthe, C. W., Sarma, A., Kumar, G., Sutnaga, C., Kalita, M., & Roy, P. (2019 ). Causes of treatment abandonment of pediatric cancer patients - experience in a regional cancer center in North East India. Asian Pacific Journal of Cancer Prevention, 20(4), 1133–1137. https://doi.org/10.31557/APJCP.2019.20.4.1133
Hunger, S. P., & Mullighan, Gc. (2015). Acute lymphoblastic leukemia in children. The New England Journal of Medicine, 373(1), 1541–1552. https://doi.org/10.1056/NEJMra1400972
Khazaei, Z., Goodarzi, E., Adineh, H. A., Moradi, Y., Sohrabivafa, M., Darvishi, I., & Dehghani, S. L. (2019). Epidemiology, incidence, and mortality of leukemia in children early infancy to 14 years old of age in south-central Asia: A global ecological study. Journal of Comprehensive Pediatrics, 10(1), 1–9. https://doi.org/10.5812/compreped.82258
Kulsum, D. U., Mediani, H. S., & Bangun, A. V. (2017). The Influence of Swedish Massage Therapy on the Level of Quality of Life of School-Age Leukemia Sufferers. Padjadjaran Journal of Nursing, 5(2), 113–122. https://doi.org/10.24198/jkp.v5i2.449
Lustosa de Sousa, D. W., de Almeida Ferreira, F. V., Cavalcante Félix, F. H., & de Oliveira Lopes, M. V. (2015). Acute lymphoblastic leukemia in children and adolescents: Prognostic factors and survival analysis. Revista Brasileira de Hematologia e Hemotherapya, 37(4), 223–229. https://doi.org/10.1016/j.bjhh.2015.03.009
McGaghie, W. C., Bondage, G., & Shea, J. A. (2001). Problem Statement, Conceptual Framework, and Research Question. Academic Medicine, 76(9), 920???921. https://doi.org/10.1097/00001888-200109000-00020
Mock, V., St. Ours, C., Hall, S., Bositis, A., Tillery, M., Belcher, A., Krumm, S., & McCorkle, R. (2007). Using a conceptual model in nursing research - Mitigating fatigue in cancer patients. Journal of Advanced Nursing, 58(5), 503–512. https://doi.org/10.1111/j.1365-2648.2007.04293.x
Momani, T. G., Hathaway, D. K., & Mandrell, B. N. (2016). Factors Affecting Health-Related Quality of Life in Children Undergoing Curative Treatment for Cancer: A Review of the Literature. Journal of Pediatric Oncology Nursing, 33(3), 228–240. https://doi.org/10.1177/1043454215609585
Mostert, S., Gunawan, S., van Dongen, J. A. P., van de Ven, P. M., Sitaresmi, M. N., Wolters, E. E., & Veerman, A. J. (2013). Health-care providers' perspectives on childhood cancer treatment in Manado, Indonesia. Psycho-Oncology, 22(May), 2522–2528. https://doi.org/10.1002/pon.3314
Mostert, S., Sitaresmi, M. N., Gundy, C. M., Janes, V., Sutaryo, S., & Veerman, A. J. (2010). Comparing childhood leukemia treatment before and after the introduction of a parental education program in Indonesia. Archives of Disease in Childhood, 95(1), 20–25. https://doi.org/10.1136/adc.2008.154138
Mostert, S., Sitaresmi, M. N., Gundy, C. M., & Veerman, A. J. (2008). Parental Experiences of Childhood Leukemia Treatment in Indonesia. Journal of Pediatric Hematology/Oncology, 30(10), 738–743. https://doi.org/10.1097/MPH.0b013e31817e4aad
Mwirigi, A., Dillon, R., & Raj, K. (2017). Acute leukemia. Medicine (United Kingdom), 45(5), 280–286. https://doi.org/10.1016/j.mpmed.2017.02.010
Novrianda, D., & Khairina, I. (2015). The effect of educational intervention on the quality of life of acute lymphocytic leukemia who are undergoing chemotherapy. International Journal of Research in Medical Sciences, July, S69–S73. https://doi.org/10.18203/2320-6012.ijrms20151523
Novrianda, D., Yetti, K., & Agustini, N. (2016). Factors Associated with Quality of Life in Children with Acute Lymphocytic Leukemia Undergoing Chemotherapy. Padjadjaran Journal of Nursing, v4(n1), 1–10. https://doi.org/10.24198/jkp.v4n1.1
Palagyi, A., Balane, C., Shanthosh, J., Jun, M., Bhoo-Pathy, N., Gadsden, T., Canfell, K., & Jan, S. (2021). Treatment of abandonment in children with cancer: Does a sex difference exist? A systematic review and meta-analysis of evidence from low- and middle-income countries. International Journal of Cancer, 148(4), 895–904. https://doi.org/10.1002/ijc.33279
Permatasari, E., Windiastuti, E., & Satari, H. K. (2009). Survival and prognostic factors of childhood acute lymphoblastic leukemia. Paediatrica Indonesiana, 49(6), 365–371. https://doi.org/10.14238/pi
Rata, N. S., Basit, M., & Anggraini, S. (2017). Correlation of family emotional support and level of pain in children with acute lymphoblastic leukemia due to chemotherapy (Correlation of family emotional support and level of pain in children with acute lymphoblastic leukemia). Health Dynamics Journal of Midwifery and Nursing, 8(2), 494–501. https://doi.org/10.51143/jksi.v3i1.88
Reedijk, A. M. J., Coebergh, J. W. W., de Groot-Kruseman, H. A., van der Sluis, I. M., Kremer, L. C., Karim-Kos, H. E., & Pieters, R. (2021). Progress against childhood and adolescent acute lymphoblastic leukemia in the Netherlands, 1990–2015. Leukemia, 35(4), 1001–1011. https://doi.org/10.1038/s41375-020-01024-0
Schoemann, A. M., Boulton, A. J., & Short, S. D. (2017). Determining Power and Sample Size for Simple and Complex Mediation Models. Social Psychological and Personality Science, 8(4), 379–386. https://doi.org/10.1177/1948550617715068
Siegel, R. L., Miller, K. D., Fuchs, H. E., & Jemal, A. (2022). Cancer statistics, 2022. CA: A Cancer Journal for Clinicians, 72(1), 7–33. https://doi.org/10.3322/caac.21708
Simanjorang, C., Kodim, N., & Tehuteru, E. S. (2013). Differences in 5-year survival of acute lymphoblastic leukemia and acute myeloblastic leukemia in children at the "Dharmais" Cancer Hospital, Jakarta, 1997-2008. Indonesian Journal of Cancer, 7(1), 15–21.
Sitaresmi, M. N., Mostert, S., Gundy, C. M., Ismail, D., & Veerman, A. J. (2013). A medication diary-book for pediatric patients with acute lymphoblastic leukemia in Indonesia. Pediatric Blood & Cancer, 60(February), 1593–1597. https://doi.org/10.1002/pbc.24570
Sitaresmi, M. N., Mostert, S., Gundy, C. M., Sutaryo, S., & Veerman, A. J. (2008). Health-related quality of life assessment in Indonesian childhood acute lymphoblastic leukemia. Health and Quality of Life Outcomes, 6, 1–8. https://doi.org/10.1186/1477-7525-6-96
Sitaresmi, M. N., Mostert, S., Schook, R. M., Sutaryo, S., & Veerman, A. J. (2010). Refusal and abandonment treatment in childhood acute lymphoblastic leukemia in Indonesia: An analysis of causes and consequences. Psycho-Oncology, 19(4), 361–367. https://doi.org/10.1002/pon.1578
Sjakti, H. A., Gatot, D., & Windiastuti, E. (2016). Results of Treatment of Acute Myeloblastic Leukemia in Children. Sari Pediatrics, 14(1), 40. https://doi.org/10.14238/sp14.1.2012.40-5
Sjakti, H. A., & Windiastuti, E. (2016). Patterns of Infection in Acute Myeloblastic Leukemia in Children. Sari Pediatrics, 13(6), 426. https://doi.org/10.14238/sp13.6.2012.426-30
Supriyadi, E., Widjajanto, P. H., Purwanto, I., Cloos, J., Veerman, A. J., & Sutaryo, S. (2011). Incidence of childhood leukemia in Yogyakarta, Indonesia, 1998–2009. Pediatric Blood & Cancer, 57(4), 588–593. https://doi.org/10.1002/pbc.23109
Supriyadi, E., Widjajanto, P. H., Veerman, A. J. P., Purwanto, I., Nency, Y. M., Gunawan, S., Nafianti, S., Purnomosari, D., Intansari, U. S., Westra, G., Sutaryo, & Cloos , J. (2011). Immunophenotypic patterns of childhood acute leukemias in Indonesia. Asian Pacific Journal of Cancer Prevention, 12(12), 3381–3387.
Suryani, A. E., & Syafiq, M. (2016). Living With Leukemia: A Phenomenological Study of Adolescents with Leukemia. Journal of Theory and Applied Psychology, 6(2), 78. https://doi.org/10.26740/jptt.v6n2.p78-90
Tehuteru, E. S. (2011). Overview of Remission Rates in Leukemia. Indonesian Journal Cancer Vol 5, No.4, 5(4), 4–7.
Vora, A. (2016). Childhood leukemia: An update. Paediatrics and Child Health (United Kingdom), 26(2), 51–56. https://doi.org/10.1016/j.paed.2015.10.007
Widianita, P. L., Mikarsa, H. L., & Hartiani, F. (2009). Description of the Meaning of Life in Adolescents with Leukemia. Indonesian Journal of Cancer, 3(1), 17–23. https://doi.org/10.33371/ijoc.v3i1.72
Widiaskara, I. M., Permono, B., Ugrasena, I. D., & Andarsini, M. R. (2016). Outcome of Treatment of Induction Phase of Acute Lymphoblastic Leukemia Patients in Children at Dr. Soetomo Surabaya (Outcome of induction phase of children with ALL in Dr. Soetomo Hospital, Surabaya). Sari Pediatrics, 12(2), 128. https://doi.org/10.14238/sp12.2.2010.128-34
Wijayanti, L. P., & Supriyadi, E. (2017). Prognostic Factors and Patient Survival. Indonesian Journal of Cancer, 11(4), 145–150.
Sure, R., Syarif, S., & Tehuteru, E. S. (2017). Comparison of Three Year Survival in Children with Acute Lymphoblastic Leukemia between the 2006 and 2013 Treatment Protocols. Indonesian Journal of Cancer, 11(3), 111. https://doi.org/10.33371/ijoc.v11i3.515
Downloads
Submitted
Accepted
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Siti Arifah, Autchareeya Patoomwan

This work is licensed under a Creative Commons Attribution 4.0 International License.


















