Analysis of Factors Influencing the Incidence of Urinary Incontinence in Elderly Women in Medan
DOI:
https://doi.org/10.23917/bik.v16i2.1671Keywords:
blood pressure, elderly women, incidence, labor, urinary incontinenceAbstract
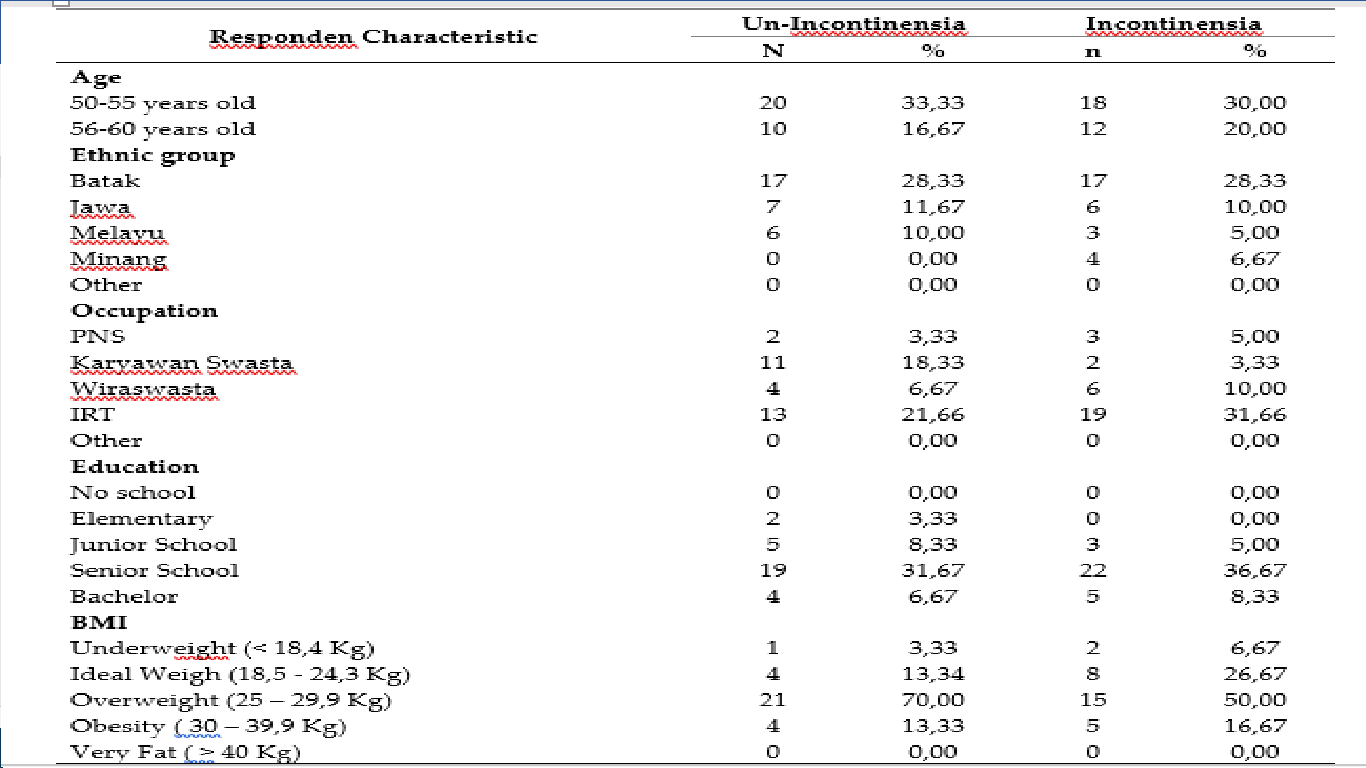
Urinary incontinence is a serious health problem that is very vulnerable to be experienced by the elderly caused by urinary disorders, especially women who can increase the risk of postpartum infection. This study used an observational analytic study with astudy design case control with aapproach. A retrospective approach was used to see how many factors were diabetes mellitus, hypertension, parity, mode of delivery, history of hysterectomy surgery, history of gynecological surgery, menopause, body mass index (BMI) and education towards the effect of urinary incontinence in the case group and control group in elderly women in Medan. The results of the study based on the results of statistical tests obtained p value > 0.05 indicating that there was no effect of increasing body weight on the incidence of urinary incontinence. In the blood sugar level variable, the p value <0.05 showed that there was an effect of blood sugar levels on the incidence of urinary incontinence with an OR = 4.375 (95% Cl; 1.320-14.504). blood pressure on the incidence of urinary incontinence with a value of OR = 4.250 (95% Cl; 0.507-9.993), the variable history of delivery obtained p value <0.05 there is an effect of mode of delivery on the incidence of urinary incontinence with an OR value of 4.190 (Cl 95%; 0.716-6.698), the parity variable obtained p value > 0.05, there was no effect of the number of parity on the incidence of urinary incontinence, the variable length of menopause obtained p value > 0.05 indicating that there was no effect of the length of menopause on the incidence of urinary incontinence, on the history of hysterectomy variable obtained p value <0.05, there is an influence between the history of hysterectomy surgery on the incidence of urinary incontinence with OR = 2.740 (95% Cl; 0.252-2.175), on the variable r gynecological history Statistical test results obtained p value > 0.05 indicating that there is no effect between the history of geniculate surgery on the incidence of urinary incontinence
Downloads
References
Almousa, S., & Bandin Van Loon, A. (2019). The prevalence of urinary incontinence in nulliparous female sportswomen: A systematic review. Journal of Sports Sciences, 37(14), 1663–1672. https://doi.org/10.1080/02640414.2019.1585312.
Corrado, B., Giardulli, B., Polito, F., Aprea, S., Lanzano, M., & Dodaro, C. (2020). The impact of urinary incontinence on quality of life: A cross-sectional study in the metropolitan city of Naples. Geriatrics (Switzerland), 5(4), 1–14. https://doi.org/10.3390/geriatrics5040096
Esparza, A. O., Tomás, M. Á. C., & Pina-Roche, F. (2018). Experiences of women and men living with urinary incontinence: A phenomenological study. Applied Nursing Research, 40(December 2017), 68–75. https://doi.org/10.1016/j.apnr.2017.12.007
Faasse, M. A., Nosnik, I. P., Diaz-Saldano, D., Hodgkins, K. S., Liu, D. B., Schreiber, J., & Yerkes, E. B.(2015). Uroflowmetry with pelvic floor electromyography: inter-rater agreement on diagnosis of pediatric non-neurogenic voiding disorders. Journal of Pediatric Urology, 11(4), 198.e1-198.e6. https://doi.org/10.1016/j.jpurol.2015.05.012
Haruna, H., Hu, X., Chu, S. K. W., Mellecker, R. R., Gabriel, G., & Ndekao, P. S. (2018). Improving sexual health education programs for adolescent students through game-based learning and gamification. International Journal of Environmental Research and Public Health, 15(9), 1–26. https://doi.org/10.3390/ijerph15092027
Holly, C. (2018). Integrative Review. Scholarly Inquiry and the DNP Capstone, 32(1), 106–112. https://doi.org/10.1891/9780826193889.0008
Juananda, D., & Febriantara, D. (2017). Urinary Incontinence in the Elderly at the Nursing Home, Riau Province. Inkontinensia Urin pada Lanjut Usia di Panti Werdha Provinsi Riau. Jurnal Kesehatan Melayu, 1(1), 20. https://doi.org/10.26891/jkm.v1i1.21.20-24
Made, D., Putrawan, I. B., & Purnami, N. K. R. (2019). Hubungan Tingkat Inkontinensia Urin dengan Derajat Depresi pada Pasien Lanjut Usia di Panti Sosial Tresna Werda Wana Seraya Denpasar. JURNAL MEDIKA UDAYANA, VOL. 8 N0 8. https://ojs.unud.ac.id/index.php/eum/article/view/51800/30736
Mardliyah, W. L. (2013). Hubungan pengetahuan perawat tentang inkontinensia urin terhadap praktik perawatan inkontinensia urin di rsu kabupaten tangerang. 1–134. https://repository.uinjkt.ac.id/dspace/bitstream/123456789/25959/1/WALIDATUL%20LAILI%20MARDLIYAH-fkik.pdf
Mostafa Elbana, H. (2018). Effect of Urinary Incontinence on Quality of Life and Self Esteem of Postmenopausal Women. American Journal of Nursing Science, 7(5), 182. https://doi.org/10.11648/j.ajns.20180705.15
Okumura, N., Kondo, T., Matsushita, K., Osugi, S., Shimokata, K., Matsudaira, K., Yamashita, K., Maeda, K., & Murohara, T. (2014). Associations of proteinuria and the estimated glomerular filtration rate with incident hypertension in young to middle-aged Japanese males. Preventive Medicine, 60, 48–54. https://doi.org/10.1016/j.ypmed.2013.12.009
Omar, D. N., Khan, R., Farooq, F., Karim, H., Ayoub, M., & Habib, U. (2015). Health Care Facilities At School; Perception of Students. The Professional Medical Journal, 22(12), 1546–1549. https://doi.org/10.17957/tpmj/15.2963
Kołodyńska, G., Zalewski, M., & Rozek-Piechura, K. (2019). Urinary incontinence in postmenopausal women - Causes, symptoms, treatment. Przeglad Menopauzalny, 18(1), 46–50. https://doi.org/10.5114/pm.2019.84157
Lu, J., Zhang, H., Liu, L., Jin, W., Gao, J., Min, M., & Fan, Y. (2021). Meta-analysis of Perinatal Pelvic Floor Muscle Training on Urinary Incontinence. Western Journal of Nursing Research, 43(6), 597–605. https://doi.org/10.1177/0193945920960779
Rijal, R., Hardianti, H., & Adliah, F. (2019).Pengaruh Pemberian Kombinasi Kegel Exercise Dan Bridging Exercise Terhadap Perubahan frekuensi Inkontinensia Urin Pada Lanjut Usia Di Yayasan Batara Hati Mulia Gowa. Jurnal Ilmiah Kesehatan Sandi Husada, 7(1), 26–29. https://doi.org/10.35816/jiskh.v7i1.67
Sari, R. D. P., Obstetri, B., Kedokteran, F., & Lampung, U. (2016). Perubahan Kekuatan Otot Dasar Panggul pada Wanita Primipara Pascapersalinan Pervaginam dan Seksio Sesaria Pelvic Floor Muscles Change in Primigravidae after Vaginal Deliveries and Cesarean Section. 1, 247–255 https://juke.kedokteran.unila.ac.id/index.php/JK/article/view/1623
Slieker-ten Hove, M. C. P., Pool-Goudzwaard, A. L., Eijkemans, M. J. C., Steegers-Theunissen, R. P. M.,Burger, C. W., & Vierhout, M. E. (2009). Pelvic floor muscle function in a general female population in relation with age and parity and the relation between voluntary and involuntary contractions of the pelvic floor musculature. International Urogynecology Journal and Pelvic Floor Dysfunction, 20(12), 1497–1504. https://doi.org/10.1007/s00192-009-0978-7
Sutarmi, Setyowati, T., & Astuti, Y. (2016). Pengaruh Latihan Kegel Terhadap Frekuensi Inkontinensia Urine Pada Lansia Di Unit Rehabilitasi Sosial Margo Mukti Rembang. Jurnal Riset Kesehatan, 5(1), 1–6. http://ejournal.poltekkessmg.ac.id/ojs/index.php/jrk
Downloads
Submitted
Accepted
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Meena Agusma, Nurmaini Nurmaini, Cholina Trisa Siregar

This work is licensed under a Creative Commons Attribution 4.0 International License.


















