Foot Reflexology and 4-7-8 Breathing Exercise as Supporting Therapy to Reduce Anxiety and Maintain Vital Signs of ICU Patients
DOI:
https://doi.org/10.23917/bik.v16i2.1936Keywords:
ICU, Foot Reflexology, 4-7-8 Breathing Training, Anxiety, Physiological ValueAbstract
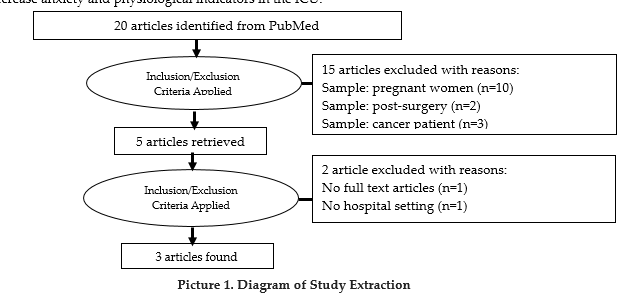
The noise of the Intensive Care Unit (ICU) equipment, the high mortality rate, the instability of other patients' conditions, and limited information increase ICU patient anxiety. Anxiety has an impact on declining health. Anxiety makes it difficult for patients to sleep, increases blood pressure values, and slows down the healing process. Management of patient anxiety is to avoid anxiety factors, use non-pharmacological and pharmacological therapies. In addition, combined pharmacological and non-pharmacological therapy is more effective in increasing patient recovery. For this reason, this study aims to evaluate the additional non-pharmacological implementation therapy of foot reflexology and 4-7-8 breathing training in patients in the ICU. The method used is a nursing practice based on evidence-based nursing implementation. The evidence-based references used are 3 international journals indexed by Scopus. The patient selection technique used purposive sampling with inclusion and exclusion criteria. Furthermore, a combination of foot reflexology intervention and 4-7-8 breathing training was given for 2 days to 3 patients. The results of the evaluation showed that there was a decrease in anxiety rates and an improvement in physiological values after being given non-pharmacological and pharmacological interventions. Improved physiological values are, blood pressure and respiratory rate. Additional non-pharmacological interventions foot reflexology and 4-7-8 breathing training reduce anxiety levels and improve the patient's physiological values.
References
Alinia-najjar, R., Bagheri-Nesami, M., Shorofi, S. A., Mousavinasab, S. N., & Saatchi, K. (2020). The effect of foot reflexology massage on burn-specific pain anxiety and sleep quality and quantity of patients hospitalized in the burn intensive care unit (ICU). Burns, 46(8), 1942–1951. https://doi.org/10.1016/j.burns.2020.04.035
Ariganjoye, F., Gibson, S., Mossad, J., Posey, A., & Sharley, J. (2023). Is therapeutic massage an effective treatment for anxiety in critically ill patients? Evidence-Based Practice, 26(4), 23–24. https://doi.org/10.1097/EBP.0000000000001803
Brathwaite, L., & Reif, M. (2019). Hypertensive Emergencies. Cardiology Clinics, 37(3), 275–286. https://doi.org/10.1016/j.ccl.2019.04.003
Brito, R. A., do Nascimento Rebouças Viana, S. M., Beltrão, B. A., de Araújo Magalhães, C. B., de Bruin, V. M. S., & de Bruin, P. F. C. (2020). Pharmacological and non-pharmacological interventions to promote sleep in intensive care units: a critical review. Sleep and Breathing, 24(1), 25–35. https://doi.org/10.1007/s11325-019-01902-7
Darbyshire, J. L., Müller-Trapet, M., Cheer, J., Fazi, F. M., & Young, J. D. (2019). Mapping sources of noise in an intensive care unit. Anaesthesia, 74(8), 1018–1025. https://doi.org/10.1111/anae.14690
Dewi, E., Nisa, N. Q., Nurmahdianingrum, S. D., & Triyono, T. (2022). Progressive Muscle Relaxation as an Effort in Reducing Anxiety for Patients with Asthma Attacks. Jurnal Berita Ilmu Keperawatan, 15(2), 185–189. https://doi.org/10.23917/bik.v15i2.18185
Dwivedi, S. (2022). The Addressing Anxiety Disorder through Indigenous Therapeutics : A Review. Dev Sanskriti Interdisciplinary International Journal, 20, 27–35. https://doi.org/10.36018/dsiij.v20i.265
Eskici İlgin, V., & Yayla, A. (2023). Effect of the 4-7-8 Breathing Technique on Pain Level and Sleep Quality of Patients After Laparoscopic Bariatric Surgery: A Randomized Controlled Study. Bariatric Surgical Practice and Patient Care. https://doi.org/10.1089/bari.2022.0044
Gál, É., Ștefan, S., & Cristea, I. A. (2021). The efficacy of mindfulness meditation apps in enhancing users’ well-being and mental health related outcomes: a meta-analysis of randomized controlled trials. Journal of Affective Disorders, 279, 131–142. https://doi.org/10.1016/j.jad.2020.09.134
Göral Türkcü, S., & Özkan, S. (2021). The effects of reflexology on anxiety, depression and quality of life in patients with gynecological cancers with reference to Watson’s theory of human caring. Complementary Therapies in Clinical Practice, 44, 101428. https://doi.org/https://doi.org/10.1016/j.ctcp.2021.101428
Götze, H., Friedrich, M., Taubenheim, S., Dietz, A., Lordick, F., & Mehnert, A. (2020). Depression and anxiety in long-term survivors 5 and 10 years after cancer diagnosis. Supportive Care in Cancer, 28(1), 211–220. https://doi.org/10.1007/s00520-019-04805-1
Inoue, S., Hatakeyama, J., Kondo, Y., Hifumi, T., Sakuramoto, H., Kawasaki, T., Nishida, O. (2019). Post‐intensive care syndrome: its pathophysiology, prevention, and future directions. Acute Medicine & Surgery, 6(3), 233–246. https://doi.org/10.1002/ams2.415
Jayanthi, J. K., & Hudiyawati, D. (2019). Therapy to improve sleep quality in ICU patients. Jurnal Berita Ilmu Keperawatan; Vol. 12, No. 2, 2019. https://doi.org/10.23917/bik.v12i2.11599
Johnson, H. M. (2019). Anxiety and Hypertension: Is There a Link? A Literature Review of the Comorbidity Relationship Between Anxiety and Hypertension. Current Hypertension Reports, 21(9), 66. https://doi.org/10.1007/s11906-019-0972-5
Khajian Gelogahi, Z., Aghebati, N., Mazloum, S. R., & Mohajer, S. (2018). Effectiveness of Nurse’s Intentional Presence as a Holistic Modality on Depression, Anxiety, and Stress of Cardiac Surgery Patients. Holistic Nursing Practice, 32(6). Retrieved from https://journals.lww.com/hnpjournal/Fulltext/2018/11000/Effectiveness_of_Nurse_s_Intentional_Presence_as_a.4.aspx
Khan, F., Amatya, B., Bensmail, D., & Yelnik, A. (2019). Non-pharmacological interventions for spasticity in adults: An overview of systematic reviews. Annals of Physical and Rehabilitation Medicine, 62(4), 265–273. https://doi.org/10.1016/j.rehab.2017.10.001
Konkani, A., & Oakley, B. (2012). Noise in hospital intensive care units—a critical review of a critical topic. Journal of Critical Care, 27(5), 522.e1-522.e9. https://doi.org/10.1016/j.jcrc.2011.09.003
Leutualy, V., Madiuw, D., Tasijawa, F. A., Sumah, D. F., Manuhutu, F., & Maelissa, S. (2022). Non-pharmacology Interventions on Pain in Critically Ill Patient: A Scoping Review. Open Access Macedonian Journal of Medical Sciences, 10(F), 182–189. https://doi.org/10.3889/oamjms.2022.7985
Miranda-Ackerman, R. C., Lira-Trujillo, M., Gollaz-Cervantez, A. C., Cortés-Flores, A. O., Zuloaga-Fernández del Valle, C. J., García-González, L. A., … González-Ojeda, A. (2020). Associations between stressors and difficulty sleeping in critically ill patients admitted to the intensive care unit: a cohort study. BMC Health Services Research, 20(1), 631. https://doi.org/10.1186/s12913-020-05497-8
Mutiah, S., & Dewi, E. (2022). Penggunaan Terapi Audio Murotal Al-Qur’an dan Efeknya terhadap Status Hemodinamik Pasien di dalam Perawatan Intensif: Tinjauan Pustaka. Jurnal Keperawatan, 14(2 SE-), 473–480. Retrieved from http://journal2.stikeskendal.ac.id/index.php/keperawatan/article/view/191
Pour-Ghaz, I., Manolukas, T., Foray, N., Raja, J., Rawal, A., Ibebuogu, U. N., & Khouzam, R. N. (2019). Accuracy of non-invasive and minimally invasive hemodynamic monitoring: where do we stand? Annals of Translational Medicine, 7(17), 421–421. https://doi.org/10.21037/atm.2019.07.06
Rahman, A., Chang, Y., Dong, J., Conroy, B., Natarajan, A., Kinoshita, T., Xu-Wilson, M. (2021). Early prediction of hemodynamic interventions in the intensive care unit using machine learning. Critical Care, 25(1), 388. https://doi.org/10.1186/s13054-021-03808-x
Ren, J., & Crowley, S. D. (2019). Role of T-cell activation in salt-sensitive hypertension. American Journal of Physiology-Heart and Circulatory Physiology, 316(6), H1345–H1353. https://doi.org/10.1152/ajpheart.00096.2019
Rezaei, M., Naseri-Salahshour, V., Rafiei, F., Mohagheghi, F., & Sajadi, M. (2022). Effect of Foot Reflexology on Anxiety in Women with Breast Cancer: A Randomized-controlled Trial. Evidence Based Care, 11(4), 33–39. https://doi.org/10.22038/ebcj.2021.59779.2550
Rios, P., Cardoso, R., Morra, D., Nincic, V., Goodarzi, Z., Farah, B., … Tricco, A. C. (2019). Comparative effectiveness and safety of pharmacological and non-pharmacological interventions for insomnia: an overview of reviews. Systematic Reviews, 8(1), 281. https://doi.org/10.1186/s13643-019-1163-9
Rusch, H. L., Rosario, M., Levison, L. M., Olivera, A., Livingston, W. S., Wu, T., & Gill, J. M. (2019). The effect of mindfulness meditation on sleep quality: a systematic review and meta-analysis of randomized controlled trials. Annals of the New York Academy of Sciences, 1445(1), 5–16. https://doi.org/10.1111/nyas.13996
Sabeti, F., Mohammadpour, M., Pouraboli, B., Tahmasebi, M., & Hasanpour, M. (2021). Health Care Providers’ Experiences of the Non-Pharmacological Pain and Anxiety Management and Its Barriers in the Pediatric Intensive Care Units. Journal of Pediatric Nursing, 60, e110–e116. https://doi.org/10.1016/j.pedn.2021.07.026
Sandvik, R. K., Olsen, B. F., Rygh, L.-J., & Moi, A. L. (2020). Pain relief from nonpharmacological interventions in the intensive care unit: A scoping review. Journal of Clinical Nursing, 29(9–10), 1488–1498. https://doi.org/10.1111/jocn.15194
Shdaifat, S. A., & Al Qadire, M. (2022). Anxiety and depression among patients admitted to intensive care. Nursing in Critical Care, 27(1), 106–112. https://doi.org/10.1111/nicc.12536
Tarazona-Alvarez, P., Pellicer-Chover, H., Tarazona-Alvarez, B., Penarrocha-Oltra, D., & Penarrocha-Diago, M. (2019). Hemodynamic variations and anxiety during the surgical extraction of impacted lower third molars. Journal of Clinical and Experimental Dentistry, 11(1), 0–0. https://doi.org/10.4317/jced.55294
Thapa, P., & Farber, D. L. (2019). The Role of the Thymus in the Immune Response. Thoracic Surgery Clinics, 29(2), 123–131. https://doi.org/10.1016/j.thorsurg.2018.12.001
Won, E., & Kim, Y.-K. (2020). Neuroinflammation-Associated Alterations of the Brain as Potential Neural Biomarkers in Anxiety Disorders. International Journal of Molecular Sciences, 21(18), 6546. https://doi.org/10.3390/ijms21186546
Yau, K. K.-Y., & Loke, A. Y. (2021). Effects of diaphragmatic deep breathing exercises on prehypertensive or hypertensive adults: A literature review. Complementary Therapies in Clinical Practice, 43, 101315. https://doi.org/10.1016/j.ctcp.2021.101315
Downloads
Submitted
Accepted
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Riska Cahyani Zahra, Enita Dewi, Neny Marumpy

This work is licensed under a Creative Commons Attribution 4.0 International License.


















