Barriers To Healthcare Access: Examining Travel Time, Waiting Times, And Service Costs in Indonesia Primary Health Care
DOI:
https://doi.org/10.23917/bik.v18i2.9068Keywords:
cost, healthcare access, primary care, waiting time, trevel timeAbstract
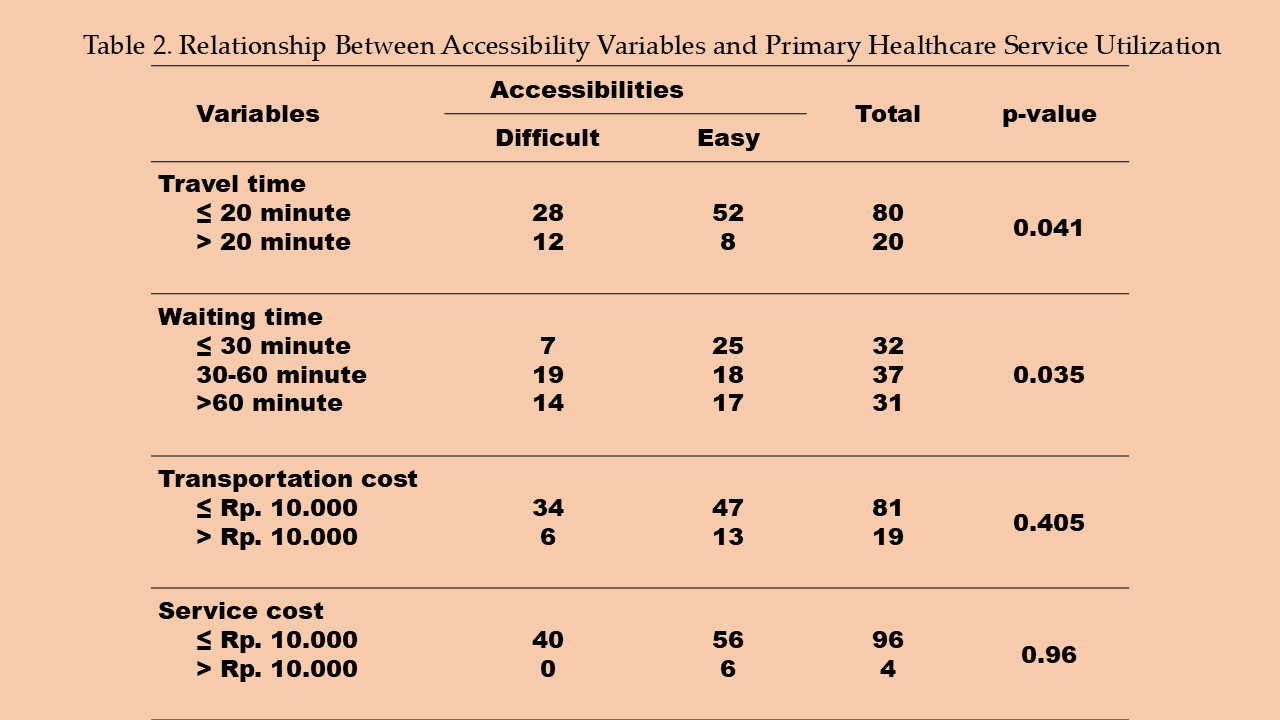
Access to primary health care in Indonesia faces significant challenges, including long travel times, high transportation costs, and poor quality of care due to a lack of health workers. These factors contribute to delays in treatment and increase the risk of severe health outcomes. Additionally, out-of-pocket expenses not covered by the national insurance program are major barriers, particularly for low-income families. To analyze the relationship between travel time, waiting time, transportation costs, service fees and access to health services. A cross-sectional study conducted in Banyumas district during May–June 2022 with 100 randomly selected adult respondents. Data were collected using a validated structured questionnaire consisting of six sections covering demographics, travel time, waiting time, transportation cost, service cost, and accessibility. Chi-Square test was used to examine relationships between the independent variables (travel time, transportation cost, service cost, and waiting time) and the dependent variable (healthcare accessibility). Travel time was significantly associated with access to health services (p = 0.041), as was waiting time (p = 0.035). However, transportation costs (p = 0.405) and service fees (p = 0.096) did not show a significant relationship. Improving transportation infrastructure and reducing waiting times through more staff and better service processes are key to enhancing healthcare access. Although transport and service costs were not statistically significant, they are still important for inclusive policy planning.
Downloads
References
Adani, Nadhila, Maulana, N., Mardani, H., Sutanto, E., Trihono, & Pattnaik, A. (2020). The Utilization of Jaminan Kesehatan Nasional (JKN) For Maternal and Neonatal Health Services in Indonesia. 1–11. https://thinkwell.global/wp-content/uploads/2022/08/Indonesia-Brief-5_MNH-gap_280722-clean.pdf
Anggraini, N. (2023). Healthcare Access and Utilization in Rural Communities of Indonesia. Journal of Community Health Provision, 3(1), 14–19. https://doi.org/10.55885/jchp.v3i1.214
Asante, D., McLachlan, C. S., Pickles, D., & Isaac, V. (2023). Understanding Unmet Care Needs of Rural Older Adults with Chronic Health Conditions: A Qualitative Study. International Journal of Environmental Research and Public Health, 20(4). https://doi.org/10.3390/ijerph20043298
Bijlmakers, L., Wientjes, M., Mwapasa, G., Cornelissen, D., Borgstein, E., Broekhuizen, H., Brugha, R., & Gajewski, J. (2019). Out-of-pocket payments and catastrophic household expenditure to access essential surgery in Malawi - A cross-sectional patient survey. Annals of Medicine and Surgery, 43, 85–90. https://doi.org/10.1016/j.amsu.2019.06.003
Cochran, A. L., McDonald, N. C., Prunkl, L., Vinella-Brusher, E., Wang, J., Oluyede, L., & Wolfe, M. (2022). Transportation barriers to care among frequent health care users during the COVID pandemic. BMC Public Health, 22(1), 1–10. https://doi.org/10.1186/s12889-022-14149-x
Cromer, K. J., Wofford, L., & Wyant, D. K. (2019). Barriers to Healthcare Access Facing American Indian and Alaska Natives in Rural America. Journal of Community Health Nursing, 36(4), 165–187. https://doi.org/10.1080/07370016.2019.1665320
Fastl, C., Arnberger, A., Gallistl, V., Stein, V. K., & Dorner, T. E. (2024). Heat vulnerability: health impacts of heat on older people in urban and rural areas in Europe. Wiener klinische Wochenschrift, 136(17-18), 507–514. https://doi.org/10.1007/s00508-024-02419-0
Idris, H. (2022). Factors associated with the choice of delivery place: A cross-sectional study in rural areas of Indonesia. Belitung Nursing Journal, 8(4), 311–315. https://doi.org/10.33546/bnj.2095
Jalloh, A., Nwosu, L. C., & Baysan, S. (2023). Evaluation of waiting time and associated factors influencing patient satisfaction levels in an outpatient department: A case study of government hospital in Sierra Leone. Science, Engineering and Health Studies. https://doi.org/10.69598/sehs.17.23050015
Jamei, E., Chan, M., Chau, H. W., Gaisie, E., & Lättman, K. (2022). Perceived Accessibility and Key Influencing Factors in Transportation. Sustainability (Switzerland), 14(17). https://doi.org/10.3390/su141710806
Jang, S. Y., Seon, J. Y., & Oh, I. H. (2020). Influencing factors of transportation costs regarding healthcare service utilization in Korea. Journal of Korean Medical Science, 35(35), 1–14. https://doi.org/10.3346/JKMS.2020.35.E290
Kaiser, N., & Barstow, C. K. (2022). Rural Transportation Infrastructure in Low-and Middle-Income Countries: A Review of Impacts, Implications, and Interventions. Sustainability (Switzerland), 14(4). https://doi.org/10.3390/su14042149
Makua, S. R., & Khunou, S. H. (2022). Nurse managers’ views regarding patients’ long waiting time at community health centers in Gauteng Province, South Africa. Belitung Nursing Journal, 8(4), 325–332. https://doi.org/10.33546/bnj.2096
Mangoma, J., Mangoma, J., & Sulistiadi, W. (2024). Island Health Crisis: Bridging Gaps in Indonesia’s Healthcare Deserts. Journal of Indonesian Health Policy and Administration, 9(2). https://doi.org/10.7454/ihpa.v9i2.1005
Mseke, E. P., Jessup, B., & Barnett, T. (2024). Impact of distance and/or travel time on healthcare service access in rural and remote areas: A scoping review. Journal of Transport and Health, 37(November 2023), 101819. https://doi.org/10.1016/j.jth.2024.101819
Nsiah, R. B., Larbi-debrah, P., Avagu, R., Yeboah, A. K., Anum-doku, S., Zakaria, S. A., Prempeh, F., Opoku, P. K., Andoono, A., Dagoe, G. E., Gmanyami, J. M., Nyarko, D., Katamani, S. K., Ganiyu, M. A., & Takramah, W. K. (2024). Mapping Health Disparities : Spatial Accessibility to Healthcare Facilities in a Rural District of Ghana Using Geographic Information Systems Techniques Mapping Health Disparities : Spatial Accessibility to Healthcare Facilities in a Rural District of Gha. September. https://doi.org/10.11648/j.ajhr.20241205.11
Nurfaiza, H., & Purwito, D. (2022). Primary Health Care Services During Pandemic. Proceedings Series on Health & Medical Sciences, 3. https://doi.org/10.30595/pshms.v3i.626
Nwagbara, U. I., Hlongwana, K. W., & Chima, S. C. (2024). Mapping evidence on the factors contributing to long waiting times and interventions to reduce waiting times within primary health care facilities in South Africa : A scoping review. 1–13. https://doi.org/10.1371/journal.pone.0299253
Pelletier, C. (2023). Inadequate Infrastructure and Resources of Rural Healthcare. Journal of Family Medicine & Medical Science Research, 12(2), 1–2. https://doi.org/10.37532/2327-4972.23.12.149
Pillai, N., Foster, N., Hanifa, Y., Ndlovu, N., Fielding, K., Churchyard, G., Chihota, V., Grant, A., & Vassall, A. (2019). Patient costs incurred by people living with HIV/AIDS prior to ART initiation in primary healthcare facilities in Gauteng, South Africa. PLoS ONE, 14. https://doi.org/10.1371/journal.pone.0210622
Rahman, A., & Pingali, P. (2024). The future of India’s social safety nets: Focus, form, and scope. https://link.springer.com/book/10.1007/978-3-031-50747-2
Ramadina, N., Ardisasmita, M. N., & Sujatmiko, B. (2021). Geographic accessibility towards primary health care in Karawang district. Kesmas, 16(3), 199–205. https://doi.org/10.21109/kesmas.v16i3.4352
Samad, S. A., Ahmad, J., Suziwana, N., Tahir, M., & Abdullah, N. C. (2023). Two Sides of the Same Coin: Accessibility and affordability for healthcare in Sabah. 227–233.
Thapa Bajgain, K., Amarbayan, M., Wittevrongel, K., McCabe, E., Naqvi, S. F., Tang, K., Aghajafari, F., Zwicker, J. D., & Santana, M. (2023). Patient-reported outcome measures used to improve youth mental health services: a systematic review. Journal of Patient-Reported Outcomes, 7(1). https://doi.org/10.1186/s41687-023-00556-0
Vedom, J., & Cao, H. (2011). Health Care Access and Regional Disparities in China. Espace Populations Sociétés, 63–78. https://api.semanticscholar.org/CorpusID:72945194
Wulandari, R. D., Laksono, A. D., Nantabah, Z. K., Rohmah, N., & Zuardin, Z. (2022). Hospital utilization in Indonesia in 2018: do urban–rural disparities exist? BMC Health Services Research, 22(1), 1–11. https://doi.org/10.1186/s12913-022-07896-5
Wulandari, R. D., Laksono, A. D., Rohmah, N., Latifah, L., & Ashar, H. (2023). Determine the Target To Increase Primary Healthcare Utilization in Indonesia’S Disadvantaged Areas. Indonesian Journal of Health Administration, 11(2), 299–310. https://doi.org/10.20473/jaki.v11i2.2023.299-310
Submitted
Accepted
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Dedy Purwito, Kris Linggardini, Arunnee Jaitieng

This work is licensed under a Creative Commons Attribution 4.0 International License.















