Community-Based Intervention for Malnutrition in Children Under Five: A Scoping Review
DOI:
https://doi.org/10.23917/bik.v18i1.6192Keywords:
Children, Community-Based Intervention, Intervention, MalnutritionAbstract
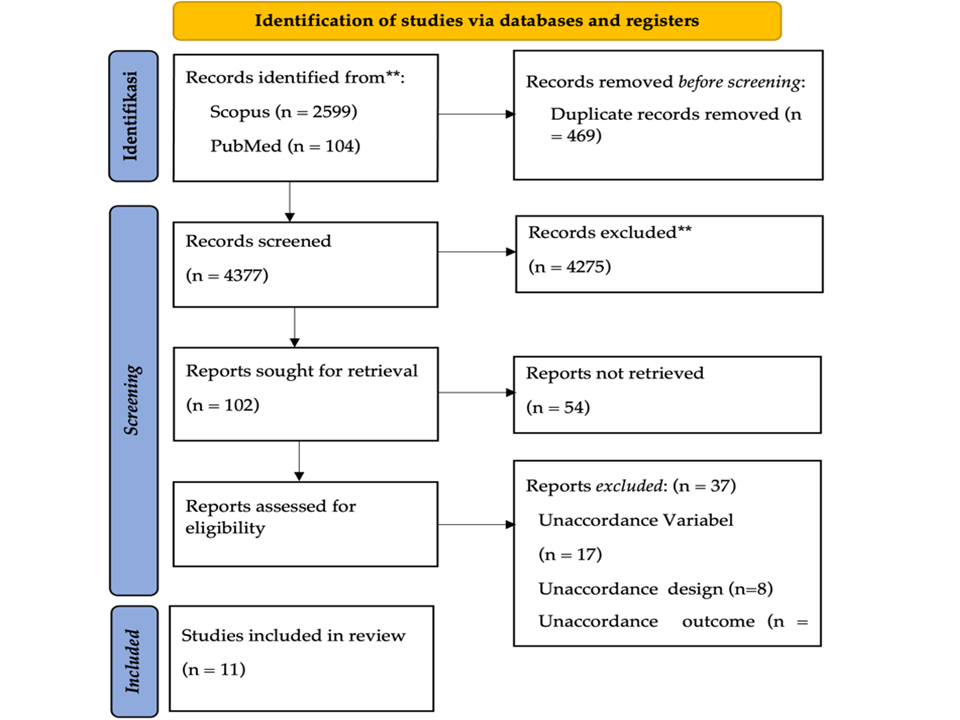
Malnutrition remains a significant global challenge, especially in developing countries. This scoping review aimed to identify community-based strategies for malnutrition in children under five. The scoping review conducted herein adhered to the methodologies outlined in conjunction with the guidelines specified in the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) extension for the scoping Reviews checklist. This study used three databases (PubMed, ProQuest, and Scopus) and included studies published between 2014-2024, with the search keywords "Intervention" or "Community-Based Intervention," “Children,” and “Malnutrition.” Results: Out of the 4846 identified articles, 11 studies were selected based on strict eligibility criteria. The results show that education, empowerment, supplementation, screening and monitoring, and other community-based interventions (home visits and meeting groups) contribute to malnutrition. The importance of community-based innovation in overcoming malnutrition in children can improve children's nutritional and health status. Program development includes increasing nutrition education, empowerment, providing adequate supplements, effective screening and monitoring to ensure the sustainability and effectiveness of community-based nutrition interventions.Downloads
References
Achmad, W. (2023). Community Empowerment Plan In Overcoming Malnutrition. Journal Sampurasun : Interdisciplinary Studies for Cultural Heritage, 9(1), 45–52. https://doi.org/10.23969/sampurasun.v9i1.7523 DOI: https://doi.org/10.23969/sampurasun.v9i1.7523
Akuu, J. A., & Amagnya, M. A. (2023). Community-based management of acute malnutrition: Implementation quality, and staff and user satisfaction with services. Journal of Taibah University Medical Sciences, 18(5), 988–996. https://doi.org/10.1016/j.jtumed.2023.02.002 PubMed: PMID: 36890797 DOI: https://doi.org/10.1016/j.jtumed.2023.02.002
Bader, B., Coenen, M., Hummel, J., Schoenweger, P., Voss, S., & Jung-Sievers, C. (2023). Evaluation of community-based health promotion interventions in children and adolescents in high-income countries: a scoping review on strategies and methods used. BMC Public Health, 23(1), 845. https://doi.org/10.1186/s12889-023-15691-y PubMed: PMID: 37165313 DOI: https://doi.org/10.1186/s12889-023-15691-y
Bidira, K., Tamiru, D., & Belachew, T. (2022). Effect of community‐based nutritional education on dietary diversity and consumption of animal‐source foods among rural preschool‐aged children in the Ilu Abba Bor zone of southwest Ethiopia: Quasi‐experimental study. Maternal & Child Nutrition, 18(4). https://doi.org/10.1111/mcn.13394 PubMed: PMID: 35758010 DOI: https://doi.org/10.1111/mcn.13394
Chapman, A. J., Ebido, C. C., Tening, R. N., Huang, Y., Sougou, N. M., Kolopaking, R., … Harder, M. K. (2024). Creating culturally-informed protocols for a stunting intervention using a situated values-based approach (WeValue InSitu): a double case study in Indonesia and Senegal. BMC Public Health, 24(1), 987. https://doi.org/10.1186/s12889-024-18485-y PubMed: PMID: 38589810 DOI: https://doi.org/10.1186/s12889-024-18485-y
De, P., & Chattopadhyay, N. (2019). Effects of malnutrition on child development: Evidence from a backward district of India. Clinical Epidemiology and Global Health, 7(3), 439–445. https://doi.org/10.1016/j.cegh.2019.01.014 DOI: https://doi.org/10.1016/j.cegh.2019.01.014
Ehlen, S., & Rehaag, R. (2018). Analyse integrierter Gesamtansätze kommunaler Gesundheitsförderung für Kinder. Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz, 61(10), 1260–1269. https://doi.org/10.1007/s00103-018-2809-9 DOI: https://doi.org/10.1007/s00103-018-2809-9
Gelli, A., Margolies, A., Santacroce, M., Roschnik, N., Twalibu, A., Katundu, M., … Ruel, M. (2018). Using a Community-Based Early Childhood Development Center as a Platform to Promote Production and Consumption Diversity Increases Children’s Dietary Intake and Reduces Stunting in Malawi: A Cluster-Randomized Trial. Journal of Nutrition, 148(10), 1587–1597. https://doi.org/10.1093/jn/nxy148 PubMed: PMID: 30204916 DOI: https://doi.org/10.1093/jn/nxy148
Hussain, D., & Biswas, B. (2024). Understanding the impact of socio-economic factors on child malnutrition in India with an emphasis on no-toilet facilities: Evidence from national family health surveys. GeoJournal, 89(1). https://doi.org/10.1007/s10708-024-11028-3 DOI: https://doi.org/10.1007/s10708-024-11028-3
Hussain, I., Habib, A., Ariff, S., Khan, G. N., Rizvi, A., Channar, S., … Soofi, S. B. (2021). Effectiveness of management of severe acute malnutrition (SAM) through community health workers as compared to a traditional facility-based model: a cluster randomized controlled trial. European Journal of Nutrition, 60(7), 3853–3860. https://doi.org/10.1007/s00394-021-02550-y PubMed: PMID: 33880645 DOI: https://doi.org/10.1007/s00394-021-02550-y
Juarez, M., Dionicio, C., Sacuj, N., Lopez, W., Miller, A. C., & Rohloff, P. (2021). Community-Based Interventions to Reduce Child Stunting in Rural Guatemala: A Quality Improvement Model. International Journal of Environmental Research and Public Health, 18(773), 1–13. https://doi.org/10.3390/ijerph PubMed: PMID: 33477580 DOI: https://doi.org/10.3390/ijerph18020773
Kang, Y., Kim, S., Sinamo, S., & Christian, P. (2017). Effectiveness of a community-based nutrition programme to improve child growth in rural Ethiopia: a cluster randomized trial. Maternal and Child Nutrition, 13(1). https://doi.org/10.1111/mcn.12349 PubMed: PMID: 27549570 DOI: https://doi.org/10.1111/mcn.12349
Katepa-Bwalya, M., Mukonka, V., Kankasa, C., Masaninga, F., Babaniyi, O., & Siziya, S. (2015). Infants and young children feeding practices and nutritional status in two districts of Zambia. International Breastfeeding Journal, 10(1), 5. https://doi.org/10.1186/s13006-015-0033-x PubMed: PMID: 25750656 DOI: https://doi.org/10.1186/s13006-015-0033-x
Korom, B., Malloy, M., Remmers, C., Cevilla, M., Dione, K., Papanek, P., … Nelson, D. (2023). “It’s about being healthy”; a novel approach to the socio-ecological model using family perspectives within the Latinx community. BMC Public Health, 23(1), 86. https://doi.org/10.1186/s12889-023-15005-2 PubMed: PMID: 36631786 DOI: https://doi.org/10.1186/s12889-023-15005-2
Liang, W., Xing, Y., Pang, M., Wang, D., & Yan, H. (2018). Community health education improves child health care in Rural Western China. BMC Pediatrics, 18(1). https://doi.org/10.1186/s12887-018-1084-0 DOI: https://doi.org/10.1186/s12887-018-1084-0
Mahmudiono, Segalita, & Rosenkranz. (2019). Socio-Ecological Model of Correlates of Double Burden of Malnutrition in Developing Countries: A Narrative Review. International Journal of Environmental Research and Public Health, 16(19), 3730. https://doi.org/10.3390/ijerph16193730 PubMed: PMID: 31623366 DOI: https://doi.org/10.3390/ijerph16193730
Maizuputri, S., Mutmainnah, M., & Meinarisa. (2024). Educational Packages on Breastfeeding Increase Behavior and Self-Efficacy of Mothers. Jurnal Berita Ilmu Keperawatan, 17(2), 152–161. https://doi.org/10.23917/bik.v17i2.4664 DOI: https://doi.org/10.23917/bik.v17i2.4664
McLeroy, K. R., Norton, B. L., Kegler, M. C., Burdine, J. N., & Sumaya, C. V. (2003). Community-Based Interventions. American Journal of Public Health, 93(4), 529–533. https://doi.org/10.2105/AJPH.93.4.529 DOI: https://doi.org/10.2105/AJPH.93.4.529
NB, T., GA, B., SM, A., & ME, Y. (2017). Prevalence and Major Contributors of Child Malnutrition in Developing Countries: Systematic Review and Meta-Analysis. Journal of Childhood Obesity, 02(04). https://doi.org/10.21767/2572-5394.100037 DOI: https://doi.org/10.21767/2572-5394.100037
Nwachan, M. B., Ejoh, R. A., Noumo, N. T., & Njong, C. E. (2024). The effects of nutrition and health education on the nutritional status of internally displaced schoolchildren in Cameroon: a randomized controlled trial. Journal of Nutritional Science, 13, e15. https://doi.org/10.1017/jns.2024.8 PubMed: PMID: 38572369 DOI: https://doi.org/10.1017/jns.2024.8
Pati, S., Mahapatra, S., Sinha, R., Pati, S., & Samal, S. N. (2018). Community Management of Acute Malnutrition (CMAM) in Odisha, India: A Multi-Stakeholder Perspective. Frontiers in Public Health, 6. https://doi.org/10.3389/fpubh.2018.00158 PubMed: PMID: 29971225 DOI: https://doi.org/10.3389/fpubh.2018.00158
Pavithra, G., Kumar, S. G., & Roy, G. (2019). Effectiveness of a community-based intervention on nutrition education of mothers of malnourished children in a rural coastal area of South India. Indian Journal of Public Health, 63(1), 4–9. https://doi.org/10.4103/ijph.IJPH_383_17 PubMed: PMID: 30880730 DOI: https://doi.org/10.4103/ijph.IJPH_383_17
Perdomo, C. D., Rodríguez, E. R., Magallanes, H. C., Flores Navarro, H. E., Matul Pérez, S. E., & Moyano, D. (2019). Impact of a community program for child malnutrition. Revista Chilena de Pediatria, 90(4), 411–421. https://doi.org/10.32641/rchped.v90i4.901 PubMed: PMID: 31859714 DOI: https://doi.org/10.32641/rchped.v90i4.901
Peters, L. E. R., Shannon, G., Kelman, I., & Meriläinen, E. (2022). Toward resourcefulness: pathways for community positive health. Global Health Promotion, 29(3), 5–13. https://doi.org/10.1177/17579759211051370 DOI: https://doi.org/10.1177/17579759211051370
Rahman, M., Tariqujjaman, Md., Ahmed, T., & Sarma, H. (2023). Effect of home visits by community health workers on complementary feeding practices among caregivers of children aged 6–23 months in 10 districts of Bangladesh. Frontiers in Public Health, 10. https://doi.org/10.3389/fpubh.2022.1014281 PubMed: PMID: 36777779 DOI: https://doi.org/10.3389/fpubh.2022.1014281
Roche, M. L., Marquis, G. S., Gyorkos, T. W., Blouin, B., Sarsoza, J., & Kuhnlein, H. V. (2017). A Community-Based Positive Deviance/Hearth Infant and Young Child Nutrition Intervention in Ecuador Improved Diet and Reduced Underweight. Journal of Nutrition Education and Behavior, 49(3), 196-203.e1. https://doi.org/10.1016/j.jneb.2016.10.007 PubMed: PMID: 27843127 DOI: https://doi.org/10.1016/j.jneb.2016.10.007
Rockers, P. C., Fink, G., Zanolini, A., Banda, B., Biemba, G., Sullivan, C., … Hamer, D. H. (2016). Impact of a community-based package of interventions on child development in Zambia: a cluster-randomised controlled trial. BMJ Global Health, 1, 104. https://doi.org/10.1136/bmjgh-2016 PubMed: PMID: 28588962 DOI: https://doi.org/10.1136/bmjgh-2016-000104
Saadah, N., Hasanah, U., & Yulianto, B. (2022). Mother Empowerment Model in Stunting Prevention and Intervention through Stunting Early Detection Training. Open Access Macedonian Journal of Medical Sciences, 10(G), 649–655. https://doi.org/10.3889/oamjms.2022.8759 DOI: https://doi.org/10.3889/oamjms.2022.8759
Setyoningsih, D. (2024). Malnutrition in Children Under Five Years and Providing Micronutrient Supplementation.JurnalKeperawatanGSH,13(1),46–55.
Shah More, N., Waingankar, A., Ramani, S., Chanani, S., Souza, V. D. ’, Pantvaidya, S., … Jayaraman, A. (2018). Community-Based Management of Acute Malnutrition to Reduce Wasting in Urban Informal Settlements of Mumbai, India: A Mixed-Methods Evaluation. Global Health: Science and Practice, 6(1), 103–127. https://doi.org/10.9745/GHSP-D-17-00182 PubMed: PMID: 29602868 DOI: https://doi.org/10.9745/GHSP-D-17-00182
Siagian, E., & Ramschie, P. A. (2024). The Influence of Mother’s Knowledge of Toddler Nutrition on Their Knowledge and Attitudes Towards Stunting. Jurnal Berita Ilmu Keperawatan, 17(2), 180–188. https://doi.org/10.23917/bik.v17i2.2835 DOI: https://doi.org/10.23917/bik.v17i2.2835
Singh, G., & Jha, A. (2024). Role of Women’s Empowerment in Improving the Nutritional Status of Children Under Five Years of Age: An Insight From the National Family Health Survey-5. Cureus. https://doi.org/10.7759/cureus.59410 PubMed: PMID: 38826598 DOI: https://doi.org/10.7759/cureus.59410
Tsabedze, B. S., & Habedi, D. S. K. (2024). Caregivers’ experiences and practices for malnourished children undergoing tuberculosis treatment in Eswatini. Health SA Gesondheid, 29. https://doi.org/10.4102/hsag.v29i0.2349 PubMed: PMID: 38726061 DOI: https://doi.org/10.4102/hsag.v29i0.2349
Umijati, S., Kardjati, S., Ismudijanto, , & Sunarjo, . (2021). Empowering Mothers through Mentoring on 6-60 Months Children’s Nutrition Care: An Effort to Prevent Child Malnutrition. Electronic Journal of General Medicine, 18(6), em324. https://doi.org/10.29333/ejgm/11311 DOI: https://doi.org/10.29333/ejgm/11311
Viajar, R. V., Dorado, J. B., Rongavilla, E. O., Caraig, G. S., & Gulay, J. J. S. (2022). Monitoring the implementation of nutrition intervention at the local level. Evaluation and Program Planning, 91, 102047. https://doi.org/10.1016/j.evalprogplan.2022.102047 PubMed: PMID: 35033960 DOI: https://doi.org/10.1016/j.evalprogplan.2022.102047
Wang, J., Chang, S., Zhao, L., Yu, W., Zhang, J., Man, Q., … Yin, S. A. (2017). Effectiveness of community-based complementary food supplement (Yingyangbao) distribution in children aged 6-23 months in poor areas in China. PLoS ONE, 12(3). https://doi.org/10.1371/journal.pone.0174302 PubMed: PMID: 28319154 DOI: https://doi.org/10.1371/journal.pone.0174302
WHO. (2023). Levels and trends in child malnutrition. World Health Organization.
Yunitasari, E., Rahayu, M., & Kurnia, I. D. (2020). The effects of lecture, brainstorming, demonstration (CBD) to mother’s knowledge, attitude, and behavior about stunting prevention on toddlers. Systematic Reviews in Pharmacy, 11(6), 1131–1136. https://doi.org/10.31838/srp.2020.6.163
Zhang, Z., Li, F., Hannon, B. A., Hustead, D. S., Aw, M. M., Liu, Z., … Huynh, D. T. T. (2021). Effect of Oral Nutritional Supplementation on Growth in Children with Undernutrition: A Systematic Review and Meta-Analysis. Nutrients, 13(9), 3036. https://doi.org/10.3390/nu13093036 PubMed: PMID: 34578914 DOI: https://doi.org/10.3390/nu13093036
Zsakai, A., Annar, D., Koronczai, B., Molnar, K., Varro, P., Toth, E., … Muzsnai, A. (2023). A new monitoring system for nutritional status assessment in children at home. Scientific Reports, 13(1), 4155. https://doi.org/10.1038/s41598-023-30998-x PubMed: PMID: 36914729 DOI: https://doi.org/10.1038/s41598-023-30998-x
Submitted
Accepted
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Vira Amelia, Yuni Sufyanti Arief, Sylvia Dwi Wahyuni

This work is licensed under a Creative Commons Attribution 4.0 International License.


















