The Impact Of Covid-19 on Homecare Workforce : An Analytical Review
DOI:
https://doi.org/10.23917/bik.v16i1.1511Keywords:
covid-19, homecare, nurse jobAbstract
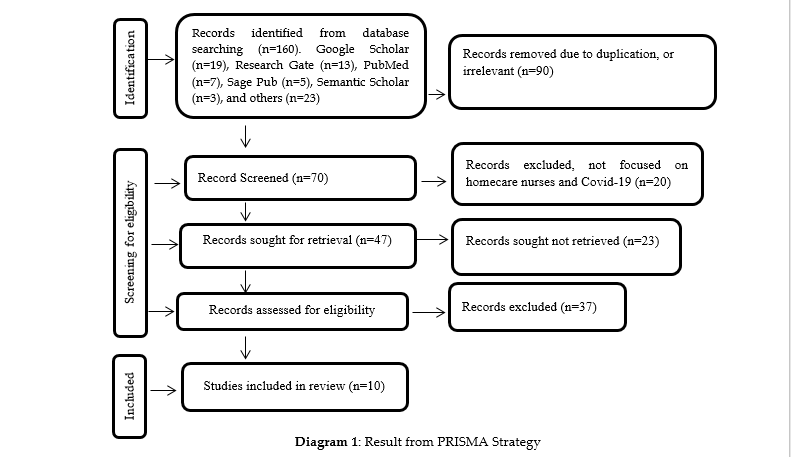
The prevalence of Covid-19 patients’ visits at health care centers in the past one and a half years has resulted in an increase in the need for a nurses workforce. Ironically, on the other hand, there is a decrease in the demand and supply of homecare nurses. This study aims to explore the impact of Covid-19 on homecare nurses and offer solutions in the form of maximizing the role of homecare nurses in the pandemic era by using a document review. The study used an analytical review with a descriptive design. The literature was drawn from Google Scholar, ResearchGate, Pubmed, SagePub, and Semantic Scholar. With the PRISMA analysis strategy, the documents in the database (n=160), which deserve to be reviewed (n=47), and those that meet the requirements for review (n=10). The output: the pandemic caused a shortage of nurses and a moderate level of stress among nurses, where agencies experienced a decrease in demand for homecare nurses. The conclusion of this research is to maximize the role of homecare nurses in the pandemic era, it is necessary to have specific guidelines or protocols regarding COVID-19 prevention and management of homecare or for a long-term care system.
Downloads
References
Al Thobaity, A., & Alshammari, F. (2020). Nurses on the Frontline against the COVID-19 Pandemic: An Integrative Review. Dubai Medical Journal, 3(3), 87–92. https://doi.org/10.1159/000509361
Allobaney, N. F., Nashwan, A. J., & Mohamed, A. S. (2020). Nursing Research during COVID-19 Pandemic?: A Scoping Review. Nursing, October. https://doi.org/10.4236/ojn.2020.1010066
Andrade, A. M., Silva, K. L., Seixas, C. T., & Braga, P. P. (2017). Nursing practice in home care: an integrative literature review. Revista Brasileira de Enfermagem, 70(1), 210–219. https://doi.org/10.1590/0034-7167-2016-0214
Bellanti, F., Buglio, A. Lo, Capuano, E., Dobrakowski, M., Kasperczyk, A., Kasperczyk, S., Ventriglio, A., & Vendemiale, G. (2021). Factors related to nurses’ burnout during the first wave of coronavirus disease-19 in a university hospital in italy. International Journal of Environmental Research and Public Health, 18(10). https://doi.org/10.3390/ijerph18105051
Bennett, L., Honeyman, M., & Bottery, S. (2018). New Models of Home Care. The King’s Fund, December, 58. https://www.kingsfund.org.uk/sites/default/files/2018-12/New-models-of-home-care.pdf
Burton, E., Senior, I. C. N., & Advisor, P. (2021). ICN Report 74 th World Health Assembly & impact in global health policy making. July.
Canadian Home Care Association, Canada, T. C. of F. P. of C., & The Canadian Nurses Association. (2016). Better home care in Canada.
Clarke, S. P., Raphael, C., & Disch, J. (2008). Challenges and Directions for Nursing in the Pay-for-Performance Movement. Policy, Politics, & Nursing Practice, 9(2), 127–134. https://doi.org/10.1177/1527154408320419
Cui, S., Jiang, Y., Shi, Q., Zhang, L., Kong, D., Qian, M., & Chu, J. (2021). Impact of covid-19 on anxiety, stress, and coping styles in nurses in emergency departments and fever clinics: A cross-sectional survey. Risk Management and Healthcare Policy, 14, 585–594. https://doi.org/10.2147/RMHP.S289782
de los Santos, J. A. A., & Labrague, L. J. (2020). Impact of COVID-19 on the psychological well-being and turnover intentions of frontline nurses in the community: A cross-sectional study in the Philippines. MedRxiv, January. https://doi.org/10.1101/2020.08.05.20167411
Genet, N., Boerma, W. G., Kringos, D. S., Bouman, A., Francke, A. L., Fagerström, C., Melchiorre, M., Greco, C., & Devillé, W. (2011). Home care in Europe: A systematic literature review. BMC Health Services Research, 11(1), 207. https://doi.org/10.1186/1472-6963-11-207
Health, M. of. (2014). Ministry of Health regulations regarding clinics. Statutary, 1(hal 140), 43. http://www.springer.com/series/15440%0Apapers://ae99785b-2213-416d-aa7e-3a12880cc9b9/Paper/p18311
Hukumonline.com. (2020). Government Regulation No 21 of 2020 concerning Large-Scale National Restrictions. 2019, 1–5.
ICN. (2020). The Global Nursing shortage and Nurse Retention. Nursing, 13–17.
ICN. (2021). International Council of Nurses Covid-19 Update (Issue January).
Karim, U. N., & Lubis, E. (2017). Quality of Life of Stroke Patients in Palliative Homecare. Jurnal Ners Dan Kebidanan Indonesia, 5(1), 42. https://doi.org/10.21927/jnki.2017.5(1).42-50
Kemenkes. (2020). Regulation of the Minister of Health of the Republic of Indonesia Number 12 of 2020 Concerning Hospital Accreditation With the Grace of God Almighty Minister of Health of the Republic of Indonesia. Orphanet Journal of Rare Diseases, 21(1), 1–9.
Koirala, A., Joo, Y. J., Khatami, A., Chiu, C., & Britton, P. N. (2020). Vaccines for COVID-19: The current state of play. Paediatric Respiratory Reviews, 35(July), 43–49. https://doi.org/10.1016/j.prrv.2020.06.010
Lee, C., Kwak, S., & Kim, J. (2021). Controlling COVID-19 outbreaks with financial incentives. International Journal of Environmental Research and Public Health, 18(2), 1–13. https://doi.org/10.3390/ijerph18020724
Lumeng, J. C., Chavous, T. M., Lok, A. S., Sen, S., Wigginton, N. S., & Cunningham, R. M. (2020). A risk–benefit framework for human research during the COVID-19 pandemic. Proceedings of the National Academy of Sciences of the United States of America, 117(45), 27749–27753. https://doi.org/10.1073/pnas.2020507117
Maharani, R., Yusyah, P., Setyawati, M. B., & Sekar, A. (2022). Family Caregiver Burden of Elderly with Dementia?: A Literature Review. 15(1), 93–103.
Maxton, F., Darbyshire, P., & Thompson, D. R. (2020). Research nurses rising to the challenges of COVID-19. Nursing, January 2021. https://doi.org/10.1111/jocn.15504
Nelson, J. A., & Folbre, N. (2006). Why a well-paid nurse is a better nurse. Nursing Economics, 24(3), 127–130.
Nugroho, C., Wiseno, B., Timur, J., & Penyakit, K. (2020). Analysis of Home Care Services As Patient Expectation During Covid-19. 27–30.
P S, J., Ramawat, V. K., K, S., A, S., & Ramawat, Y. (2020). Perceived Stress Among Nurses During Covid-19 Outbreak. GFNPSS-International Journal of Multidisciplinary Research, 1(3), 103. https://doi.org/10.46376/ijmr/1.3.2020.103-107
Sama, S. R., Quinn, M. M., Galligan, C. J., Karlsson, N. D., Gore, R. J., Kriebel, D., Prentice, J. C., Osei-Poku, G., Carter, C. N., Markkanen, P. K., & Lindberg, J. E. (2021). Impacts of the COVID-19 Pandemic on Home Health and Home Care Agency Managers, Clients, and Aides: A Cross-Sectional Survey, March to June, 2020. Home Health Care Management and Practice, 33(2), 125–129. https://doi.org/10.1177/1084822320980415
Sani T.P.; Tan M; Rustandi K.K.; Turana Y. (2020). The COVID-19 Long-Term Care situation in Indonesia. International Long-Term Care Policy Network, May, 1–16.
Silalahi, R. D., & Purba, J. M. (2022). Nurse's Experience in Caring for Diabetic Wounds During the COVID-19 Pandemic in Medan City. 15(1), 43–57.
Silitonga, T. R., & Tarigan, M. (2022). The Experience of Nurses Who Do Not Treat Covid-19 Patients at Medan City Hospital. Jurnal Berita Ilmu Keperawatan, 15(1), 58–70.
Sinaga, J., Amila, A., & Sembiring, E. (2018). Mutiara Home Care. Jurnal Pengabdian Kepada Masyarakat, 23(4), 440. https://doi.org/10.24114/jpkm.v23i4.8605
Sumardin et al. (2020). Home Care Services for Elderly Patients?: Keperawatan, 11(2), 216–225.
Syahrial. (2020). Dampak Covid-19 terhadap Tenaga Kerja. Ners, 4(23), 21–29.
The BrightStar Care. (n.d.). Homecare Planning Guide.
Tukayo, I. J. H., Kr Maay, J., Sirait, P., & Nugroho, H. S. W. (2020). The Stress Level and its Effect on Learning Achievements of Health Students due to Corona Pandemic in Indonesia. Systematic Reviews in Pharmacy, 11(12), 2375–2379.
United Nations. (2020). Policy Brief: The Impact of COVID-19 on older persons. United Nations Sustainable Development Group, 5, 1–16.
Victor Tseng. (2021). COVID-19 Healthcare Delivery Impacts. Tracie, April 2021, 1–16. https://twitter.com/VectorSting/status/1244671755781898241%0Ahttps://files.asprtracie.hhs.gov/documents/covid-19-healthcare-delivery-impacts.pdf.
WHO. (2020a). Community based Health Services in Covid-19 Pandemic Context.
WHO. (2020b). Health workforce policy and management in the context of the COVID-19 pandemic response Interim guidance. December, 29.
Widayati, M. Y., Tamtomo, D., Adriani, R. B., Hutagaol, R., Edi Wahyudi, R., Yulianty Permanasari, V., Bender, M., Spiva, L. A., Su, W., Hites, L., Johannessen, T., Ree, E., Aase, I., Bal, R., Wiig, S., Saeed, Z., Hassan, Z., Turab, S. M., Zaidi, S. A., … Merkur, Sherry; Anna Maresso, Jonathan Cylus, E. van G. and S. L. (2015). Factors Affecting Quality of Health Service and Patient Satisfaction in Community Health Centers in North Lampung, Sumatera. Journal of Health Policy and Management, 26(1), 165–175. https://doi.org/10.26911/thejhpm.2017.02.02.08
Downloads
Submitted
Accepted
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Edison Kabak, Sarlota Auparai, Yoel Halotopo

This work is licensed under a Creative Commons Attribution 4.0 International License.