Medication Adherence and Quality of Life in Patients With Depression at Psychiatric Hospital in Surakarta, Indonesia
DOI:
https://doi.org/10.23917/pharmacon.v22i2.13964Keywords:
Depresion, Medication, Adherence, Quality of LifeAbstract
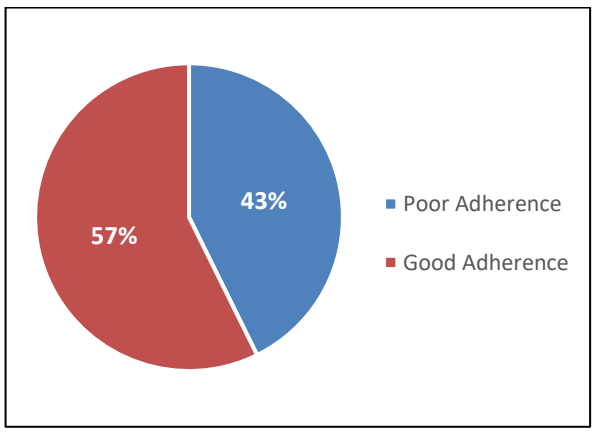
Non-adherence to depression treatment may result in elevated risk of disease development, morbidity, and premature mortality, along with a deterioration in quality of life. This study is to investigate the correlation between medication adherence and quality of life among patients with depression receiving treatment in a psychiatric hospital in Surakarta, Indonesia. This cross-sectional quantitative study on depression was undertaken at the Psychiatric Hospital in Surakarta from March to June 2025. The instruments employed were the MARS-10 and WHOQoL-BREF questionnaires, both of which were translated into Indonesian. Spearman’s rho was used to assess the correlation between medication adherence and quality-of-life ratings. SPSS 29 was used to analyse, with a p-value < 0.05 deemed significant. Of the 110 patients who participated, the majority were aged 18-35 years (51.8%), female (51.8%), had 12 years of education or more (62.7%), and were unmarried (57.3%). A majority were employed (59.1%), received treatment for 6-12 months (46.4%), and exhibited no comorbidities (90.9%). The mean treatment adherence score among patients was 8.15 ± 2.02. Sixty-three patients (57.3%) demonstrated good adherence to their medication. The correlation test results between treatment adherence and the quality of life in patients with depression indicated a statistically significant relationship (p < 0.001; r = 0.550). Increased adherence to medication correlates positively with improved quality of life in patients suffering from depression.
Downloads
References
Baeza-Velasco, C., Olié, E., Béziat, S., Guillaume, S., & Courtet, P. (2019). Determinants of suboptimal medication adherence in patients with a major depressive episode. Depression and Anxiety, 36(3), 244–251. https://doi.org/10.1002/da.22852
Bhowmik, D., Kumar, K. P. S., Srivastava, S., Paswan, S., & Dutta, A. S. (2012). Depression—Symptoms, Causes, Medications and Therapies. The Pharma Innovation Journal, 1(3), 37–51.
Cao, W., Guo, C., Ping, W., Tan, Z., Guo, Y., & Zheng, J. (2016). A Community-Based Study of Quality of Life and Depression among Older Adults. International Journal of Environmental Research and Public Health, 13(7), 693. https://doi.org/10.3390/ijerph13070693
Charan, J., & Biswas, T. (2013). How to Calculate Sample Size for Different Study Designs in Medical Research? Indian Journal of Psychological Medicine, 35(2), 121–126. https://doi.org/10.4103/0253-7176.116232
DepKes RI. (2019). Laporan Nasional Riskesdas 2018, Kementerian Kesehatan RI. Kementerian Kesehatan Republik Indonesia.
Ganesan, S., Selvaraj, N., Dass, V. K., Jayabalan, N., Rajamohammad, M. A., & Anandan, I. (2019). Assessment of drug attitude, medication adherence and quality of life among psychiatric patients in South Indian population: A cross sectional study. International Journal of Basic & Clinical Pharmacology, 8(1), 61–67. https://doi.org/10.18203/2319-2003.ijbcp20185159
Global Burden Disease. (2021). Global Burden of Disease (GBD). https://www.healthdata.org/research-analysis/gbd
Gureje, O., Kola, L., Afolabi, E., & Olley, B. O. (2008). Determinants of quality of life of elderly Nigerians: Results from the Ibadan Study of Ageing. African Journal of Medicine and Medical Sciences, 37(3), 239–247. https://pmc.ncbi.nlm.nih.gov/articles/PMC2820711/
Hansson, L. (2002). Quality of life in depression and anxiety. International Review of Psychiatry, 14(3), 185–189. https://doi.org/10.1080/09540260220144966
Health (UK), N. C. C. for M. (2010). The classification of depression and depression rating scales/questionnaires. In Depression in Adults with a Chronic Physical Health Problem: Treatment and Management. British Psychological Society (UK). https://www.ncbi.nlm.nih.gov/books/NBK82926/
Kalfoss, M. H., Reidunsdatter, R. J., Klöckner, C. A., & Nilsen, M. (2021). Validation of the WHOQOL-Bref: Psychometric properties and normative data for the Norwegian general population. Health and Quality of Life Outcomes, 19, 13. https://doi.org/10.1186/s12955-020-01656-x
Kumari, P., Parihar, A., Suthar, N., Nebhinani, M., & Khan, A. (2024). Drug Attitude and Medication Adherence among Patients with Psychiatric Illness: A Cross-sectional Analytical Study. Indian Journal of Psychiatric Nursing, 21(2), 108. https://doi.org/10.4103/iopn.iopn_72_23
Ministry of Health, Republic of Indonesia. (2024, May 28). Survei Kesehatan Indonesia (SKI) 2023. https://kemkes.go.id/id/survei-kesehatan-indonesia-ski-2023
Mishra, A., Kishor, M. R., & Ramesh, M. (2025). Randomized controlled trial to assess medication adherence and health-related quality of life through a collaborative pharmacist-psychiatrist approach to patient education in patients with depression in India. Frontiers in Psychiatry, 16. https://doi.org/10.3389/fpsyt.2025.1499893
Mishra, S. R., Sharma, A., Bhandari, P. M., Bhochhibhoya, S., & Thapa, K. (2015). Depression and Health-Related Quality of Life among Patients with Type 2 Diabetes Mellitus: A Cross-Sectional Study in Nepal. PLoS ONE, 10(11), e0141385. https://doi.org/10.1371/journal.pone.0141385
Munira, L., Liamputtong, P., Herman, B., & Viwattanakulvanid, P. (2025). Medication adherence, depression levels, and quality of life among young people with depression in Indonesia: A mixed method study. Social Psychiatry and Psychiatric Epidemiology, 60(7), 1731–1740. https://doi.org/10.1007/s00127-025-02819-1
Purba, F. D., Hunfeld, J. A. M., Iskandarsyah, A., Fitriana, T. S., Sadarjoen, S. S., Passchier, J., & Busschbach, J. J. V. (2018). Quality of life of the Indonesian general population: Test-retest reliability and population norms of the EQ-5D-5L and WHOQOL-BREF. PLoS ONE, 13(5), e0197098. https://doi.org/10.1371/journal.pone.0197098
Puspitasari, I. M., Sinuraya, R. K., Rahayu, C., Witriani, W., Zannah, U., Hafifah, A., Ningtyas, A. R., & Vildayanti, H. (2020).
Medication Profile and Treatment Cost Estimation Among Outpatients with Schizophrenia, Bipolar Disorder, Depression, and Anxiety Disorders in Indonesia
. Neuropsychiatric Disease and Treatment, 16, 815–828. https://doi.org/10.2147/NDT.S240058Santi, N. S., Biswal, S. B., Naik, B. N., Sahoo, J. P., & Rath, B. (2023). Quality of Life and Medication Adherence in Patients With Major Depressive Disorder: An Interim Analysis of a Randomized Study. Cureus, 15(6), e39997. https://doi.org/10.7759/cureus.39997
Semahegn, A., Torpey, K., Manu, A., Assefa, N., Tesfaye, G., & Ankomah, A. (2020). Psychotropic medication non-adherence and its associated factors among patients with major psychiatric disorders: A systematic review and meta-analysis. Systematic Reviews, 9(1), 17. https://doi.org/10.1186/s13643-020-1274-3
Sirey, J. A., Bruce, M. L., Alexopoulos, G. S., Perlick, D. A., Friedman, S. J., & Meyers, B. S. (2001). Stigma as a Barrier to Recovery: Perceived Stigma and Patient-Rated Severity of Illness as Predictors of Antidepressant Drug Adherence. Psychiatric Services, 52(12), 1615–1620. https://doi.org/10.1176/appi.ps.52.12.1615
Suryaputri, I. Y., Mubasyiroh, R., Idaiani, S., & Indrawati, L. (2021). Determinants of Depression in Indonesian Youth: Findings From a Community-based Survey. Journal of Preventive Medicine and Public Health, 55(1), 88–97. https://doi.org/10.3961/jpmph.21.113
Taherdoost, H. (2016). Validity and Reliability of the Research Instrument; How to Test the Validation of a Questionnaire/Survey in a Research. SSRN Electronic Journal. https://doi.org/10.2139/ssrn.3205040
Tang, J., & Zhang, T. (2022). Causes of the male-female ratio of depression based on the psychosocial factors. Frontiers in Psychology, 13. https://doi.org/10.3389/fpsyg.2022.1052702
Thompson, K., Kulkarni, J., & Sergejew, A. A. (2000). Reliability and validity of a new Medication Adherence Rating Scale (MARS) for the psychoses. Schizophrenia Research, 42(3), 241–247. https://doi.org/10.1016/S0920-9964(99)00130-9
WHO. (2025). WHOQOL-BREF - WHO - Quality of Life—Brief. https://novopsych.com/assessments/formulation/who-quality-of-life-brief-whoqol-bref/
Wijaya, M. C., & Kloping, Y. P. (2021). Validity and reliability testing of the Indonesian version of the eHealth Literacy Scale during the COVID-19 pandemic. Health Informatics Journal. https://doi.org/10.1177/1460458220975466
Wong, F. Y., Yang, L., Yuen, J. W. M., Chang, K. K. P., & Wong, F. K. Y. (2018). Assessing quality of life using WHOQOL-BREF: A cross-sectional study on the association between quality of life and neighborhood environmental satisfaction, and the mediating effect of health-related behaviors. BMC Public Health, 18(1), 1113. https://doi.org/10.1186/s12889-018-5942-3
World Health Organization. (2003). Adherence to Long-Term Therapies: Evidence for Action. https://www.paho.org/en/documents/who-adherence-long-term-therapies-evidence-action-2003
World Health Organization. (2022). World Mental Health Report: Transforming Mental Health for All (1st ed). WHO. https://www.who.int/publications/i/item/9789240049338