Evaluation of Antiretroviral and Tuberculosis Therapy Based on Clinical Outcomes in Patients With HIV/AIDS and Tuberculosis Co-Infection at Regional General Hospital in Denpasar
DOI:
https://doi.org/10.23917/pharmacon.v22i2.12652Keywords:
HIV/AIDS, TB co-infection, therapy evaluation, guidelines, treatment successAbstract
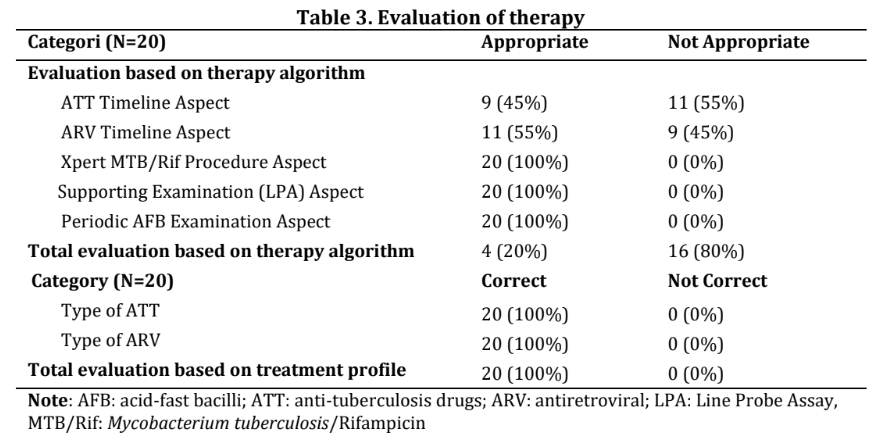
Human immunodeficiency virus and tuberculosis (HIV-TB) co-infection presents a significant challenge in Denpasar due to high incidence and complex treatment. This retrospective single-cohort study aimed to analyze the relationship between the results of therapy evaluation and the clinical outcomes in patients with HIV-TB. Secondary data from 20 HIV-TB treatment at a Regional General Hospital in Denpasar during 2022-2024 were evaluated. Fisher’s Exact test was performed to analyze the association between adherence to antiretroviral therapy (ART) and antituberculosis therapy (ATT), as per the guidelines, and their treatment success. Results showed predominance in males of productive age (60%), with cough as the most common symptom (75%), and 80% patients at HIV stage 4. All patients (N=20) received first-line ART and ATT. However, only 20% completed the treatment algorithm and 40% achieved treatment success. Although no significant association was found between treatment evaluation and success (p = 0.101), the relevant findings in this study emphasized the important role of rational drug use based on guidelines. Further studies with larger samples and a prospective approach are needed to explore additional factors affecting clinical outcomes of patients with HIV-TB undergoing therapy according to the established guidelines.
Downloads
References
Abdu, M., & Walelgn, B. (2021). Determinant factors for adherence to antiretroviral therapy among adult HIV patients at Dessie Referral Hospital, South Wollo, Northeast Ethiopia: a case–control study. AIDS Research and Therapy, 18(1), 39. https://doi.org/10.1186/s12981-021-00365-9
Ajmala, I. E., & Wulandari, L. (2015). Terapi ARV pada Penderita Ko-Infeksi TB-HIV. Jurnal Respirasi, 1(1).
Alipanah, N., Jarlsberg, L., Miller, C., Linh, N. N., Falzon, D., Jaramillo, E., & Nahid, P. (2018). Adherence interventions and outcomes of tuberculosis treatment: A systematic review and meta-analysis of trials and observational studies. PLOS Medicine, 15(7), e1002595. https://doi.org/10.1371/journal.pmed.1002595
Bisara Lolong, D., Suriani Simarmata, O., Felly Philipus Senewe Puslitbang Upaya Kesehatan Masyarakat, dan, & Litbang Kesehatan, B. (2019). Situation of Human Immunodeficiency Virus-Tuberculosis in Merauke District 2018: Threat to Productive Age. Jurnal Kesehatan Reproduksi, 10(1), 1–9. https://doi.org/10.22435/kespro.v10i1.1711.1-9
Boyd, P. S., Brown, J. B., Brown, J. D., Catazaro, J., Chaudry, I., Ding, P., Dong, X., Marchant, J., O’hern, C. T., Singh, K., Swanson, C., Summers, M. F., & Yasin, S. (2021). Correction: NMR studies of retroviral genome packaging (viruses, (2020) 12, 1115, 10.3390/v12101115). In Viruses (Vol. 13, Issue 3). MDPI AG. https://doi.org/10.3390/v13030453
Corrente, M., Park, J., Akuamoah-Boateng, H., Atanackovic, J., & Bourgeault, I. L. (2024). Work & life stress experienced by professional workers during the pandemic: a gender-based analysis. BMC Public Health, 24(1). https://doi.org/10.1186/s12889-024-18677-6
Dheda, K., Perumal, T., Moultrie, H., Perumal, R., Esmail, A., Scott, A. J., Udwadia, Z., Chang, K. C., Peter, J., Pooran, A., von Delft, A., von Delft, D., Martinson, N., Loveday, M., Charalambous, S., Kachingwe, E., Jassat, W., Cohen, C., Tempia, S., … Pai, M. (2022). The intersecting pandemics of tuberculosis and COVID-19: population-level and patient-level impact, clinical presentation, and corrective interventions. The Lancet Respiratory Medicine, 10(6), 603–622. https://doi.org/10.1016/S2213-2600(22)00092-3
Griesel, R., Zhao, Y., Simmons, B., Omar, Z., Wiesner, L., Keene, C. M., Hill, A. M., Meintjes, G., & Maartens, G. (2023). Standard-dose versus double-dose dolutegravir in HIV-associated tuberculosis in South Africa (RADIANT-TB): a phase 2, non-comparative, randomised controlled trial. The Lancet HIV, 10(7), e433–e441. https://doi.org/10.1016/S2352-3018(23)00081-4
Gupta-Wright, A., Ha, H., Abdulgadar, S., Crowder, R., Emmanuel, J., Mukwatamundu, J., Marcelo, D., Phillips, P. P. J., Christopher, D. J., Nhung, N. V., Theron, G., Yu, C., Nahid, P., Cattamanchi, A., Worodria, W., Denkinger, C. M., Thangakunam, B., Shankar, D., Ernest, V., … Yerlikaya, S. (2024). Evaluation of the Xpert MTB Host Response assay for the triage of patients with presumed pulmonary tuberculosis: a prospective diagnostic accuracy study in Viet Nam, India, the Philippines, Uganda, and South Africa. The Lancet Global Health, 12(2), e226–e234. https://doi.org/10.1016/S2214-109X(23)00541-7
Lee, H., Bea, S., Kim, J. H., Jeong, H. E., Jang, S. H., Son, H., & Shin, J.-Y. (2024). Predictors, mortality, and health outcomes of intensive phase non-adherence to a regimen in patients with drug-susceptible tuberculosis: a nationwide linkage database. Public Health, 229, 167–175. https://doi.org/10.1016/j.puhe.2024.01.021
Ministry of Health of the Republic of Indonesia. (2023). Petunjuk Teknis Kolaborasi TBC HIV (L. Luhukay & G. B. Leksono Adhi, Eds.). Kementerian Kesehatan RI.
Moyo, I., Mavhandu-Mudzusi, A. H., Lipeleke, F., & Sibindi, M. (2023). Access to HIV prevention, treatment, and care services during COVID-19 by men who have sex with men in Zimbabwe, An interpretive phenomenological analysis study. PLoS ONE, 18(4 APRIL). https://doi.org/10.1371/journal.pone.0281799
Nurita Andayani. (2023). Analisis Efektivitas Penanggulangan Tuberkulosis Paru dan Terapi Pengobatan HIV-Co-TB di Sulianti Saroso. Jurnal Ilmu Kefarmasian Indonesia, 21, 193. https://doi.org/https://doi.org/10.35814/jifi.v21i1
Patel, A., Pundkar, A., Agarwal, A., Gadkari, C., Nagpal, A. K., & Kuttan, N. (2024). A Comprehensive Review of HIV-Associated Tuberculosis: Clinical Challenges and Advances in Management. Cureus. https://doi.org/10.7759/cureus.68784
Putri, V., Botutihe, A., Jusuf, H., Arsad, N., & Penelitian, A. (2024). Analisis Faktor yang Berhubungan dengan Tingkat Kepatuhan Minum Obat Pasien Ko-Infeksi TB-HIV di Kota Gorontalo. J J Jurnal Kolaboratif Sains, 7(8), 3006–3016. https://doi.org/10.56338/jks.v7i8.5621
Rakhmandani, H., Ismaya, N. A., Hasan, M., Noersyifa, W. A., Stikes, S., Dharma, W., Tangerang, H., & Selatan, T. (2024). Evaluasi Penggunaan Obat Anti Tuberkulosis Paru Pada Pasien AIDS Di Instalasi Rawat Jalan Rumah Sakit Umum Kota Tangerang Selatan. 1(1).
Rebecca, T., Suadiatmika, D. G. M., & Margiani, N. N. (2021). Karakteristik gambaran Tuberkulosis (TB) paru pada foto toraks pasien Human Immunodeficiency Virus (HIV) tahun 2017-2021 di RSUP Sanglah, Bali, Indonesia. Intisari Sains Medis, 12(3), 934–938. https://doi.org/10.15562/ism.v12i3.1194
Sitepu, S., Sihombing, H., Nadapdap, F. M., Carol, S., Purba, A. B., Kedokteran, F., Gigi, K., & Kesehatan, I. (2024). Prevalensi Penyakit HIV/AIDS Dengan Tuberkulosis Di Rumah Sakit Royal Prima Medan Januari-Desember 2023. Action Research Literate, 8(11). https://arl.ridwaninstitute.co.id/index.php/arl
Tadesse, S. E., Zerga, A. A., Mekonnen, T. C., Tadesse, A. W., Hussien, F. M., Feleke, Y. W., Anagaw, M. Y., & Ayele, F. Y. (2022). Burden and Determinants of Anemia among Under-Five Children in Africa: Systematic Review and Meta-Analysis. In Anemia (Vol. 2022). Hindawi Limited. https://doi.org/10.1155/2022/1382940
Tesfahuneygn, G., Medhin, G., & Legesse, M. (2015). Adherence to Anti-tuberculosis treatment and treatment outcomes among tuberculosis patients in Alamata District, northeast Ethiopia. BMC Research Notes, 8(1). https://doi.org/10.1186/s13104-015-1452-x
WHO. (2016). The Use of Antiretroviral Drugs for Treating and Preventing HIV Infection 2016 ( margaret chan, Ed.; 2nd ed., Vol. 2). World Health Organization.
WHO. (2021). Consolidated Guidelines on HIV Prevention, Testing, Treatment, Service Delivery and Monitoring : Recommendations for a Public Health Approach (Vol. 2). World Health Organization.
WHO. (2025). WHO Consolidated Guidelines on Tuberculosis. Module 6: Tuberculosis and Comorbidities (2nd ed.). World Health Organization.